Understanding Status Epilepticus in Cats
Status epilepticus is a life-threatening neurological emergency in cats characterized by prolonged or recurrent seizures without full recovery in between. Unlike brief, isolated episodes, this condition can lead to brain damage, overheating, or even death if not treated immediately. While seizures in cats are less common than in dogs, status epilepticus demands urgent veterinary care and owner awareness. Recognizing the signs early and acting swiftly can make all the difference in your cat’s outcome. With expert insight and prompt intervention, many cats can stabilize and return to a good quality of life.
What Exactly Is Status Epilepticus in Cats?
Status epilepticus occurs when a seizure lasts longer than five minutes—or when multiple seizures happen in rapid succession without the cat regaining consciousness between them. This neurological crisis disrupts normal brain function and requires emergency medical treatment to stop the electrical storm in the brain.
- Prolonged Seizure Activity:
A single seizure lasting more than five minutes qualifies as status epilepticus and is considered a medical emergency. - Cluster Seizures Without Recovery:
Even if each seizure is short, if your cat doesn’t fully wake up or regain normal behavior between episodes, it’s still status epilepticus. - Loss of Consciousness and Control:
Cats in status epilepticus often collapse, paddle their legs, drool excessively, and may lose bladder or bowel control. - Risk of Secondary Complications:
Prolonged seizures can cause hyperthermia (dangerously high body temperature), respiratory distress, and brain swelling. - Not a Diagnosis—But a Symptom:
Status epilepticus signals an underlying condition like toxin exposure, brain tumor, liver failure, or idiopathic epilepsy.
Immediate veterinary intervention is crucial—every minute counts in minimizing brain injury and stabilizing your cat.
Common Causes Behind This Neurological Emergency
While the seizure itself is the visible crisis, the root cause determines long-term management and prognosis. Identifying potential triggers helps guide treatment and prevent recurrence.
- Toxin Exposure:
Ingestion of lilies, permethrin (in dog flea products), antifreeze, or certain human medications can trigger severe seizures. - Metabolic Disorders:
Liver disease (hepatic encephalopathy), kidney failure, or low blood sugar disrupt brain chemistry and provoke seizures. - Intracranial Conditions:
Brain tumors, encephalitis, strokes, or head trauma can create abnormal electrical activity in the brain. - Idiopathic Epilepsy:
Though less common in cats than dogs, some cats develop epilepsy with no identifiable cause—often appearing between 1–5 years of age. - Infectious Diseases:
Feline infectious peritonitis (FIP), toxoplasmosis, or feline leukemia virus (FeLV) may affect the nervous system and lead to seizures.
Finding the underlying cause often requires advanced diagnostics, but stabilizing the cat always comes first in an emergency.
Check this guide 👉Understanding Carcinoma in Cats: Best 7 Expert Tips!
Check this guide 👉Understanding Syringomyelia in Cats: Best 7 Expert Tips!
Check this guide 👉Sebaceous Adenitis in Cats: Best 7 Expert Tips
Emergency Warning Signs | Underlying Triggers to Investigate |
|---|---|
Seizure lasting >5 minutes | Toxin ingestion (e.g., lilies, pesticides) |
Repeated seizures without recovery | Liver or kidney dysfunction |
High body temperature during episode | Brain tumor or structural abnormality |
Labored breathing or blue gums | Infection or inflammatory brain disease |
Post-ictal disorientation lasting hours | Idiopathic (genetic) epilepsy |
Immediate Actions to Take During an Episode
If your cat enters status epilepticus, your quick response can be lifesaving. Stay calm and focus on safety while preparing for urgent veterinary transport.
- Time the Seizure:
Use your phone to note exactly when the seizure starts—this information is critical for treatment decisions. - Keep the Environment Safe:
Move furniture or hard objects away to prevent injury, but do not restrain your cat or put anything in its mouth. - Cool the Body Gently (If Needed):
If the seizure lasts beyond 3–4 minutes, use a damp, cool (not cold) cloth on the paws or ears to help prevent overheating. - Avoid Loud Noises or Bright Lights:
Dim lights and minimize sound to reduce additional neurological stimulation during the episode. - Call Your Vet Immediately:
Alert the clinic en route so they can prepare IV medications like diazepam to stop the seizure upon arrival.
Never delay care—status epilepticus is not something that resolves on its own and requires emergency drugs to halt brain overactivity.
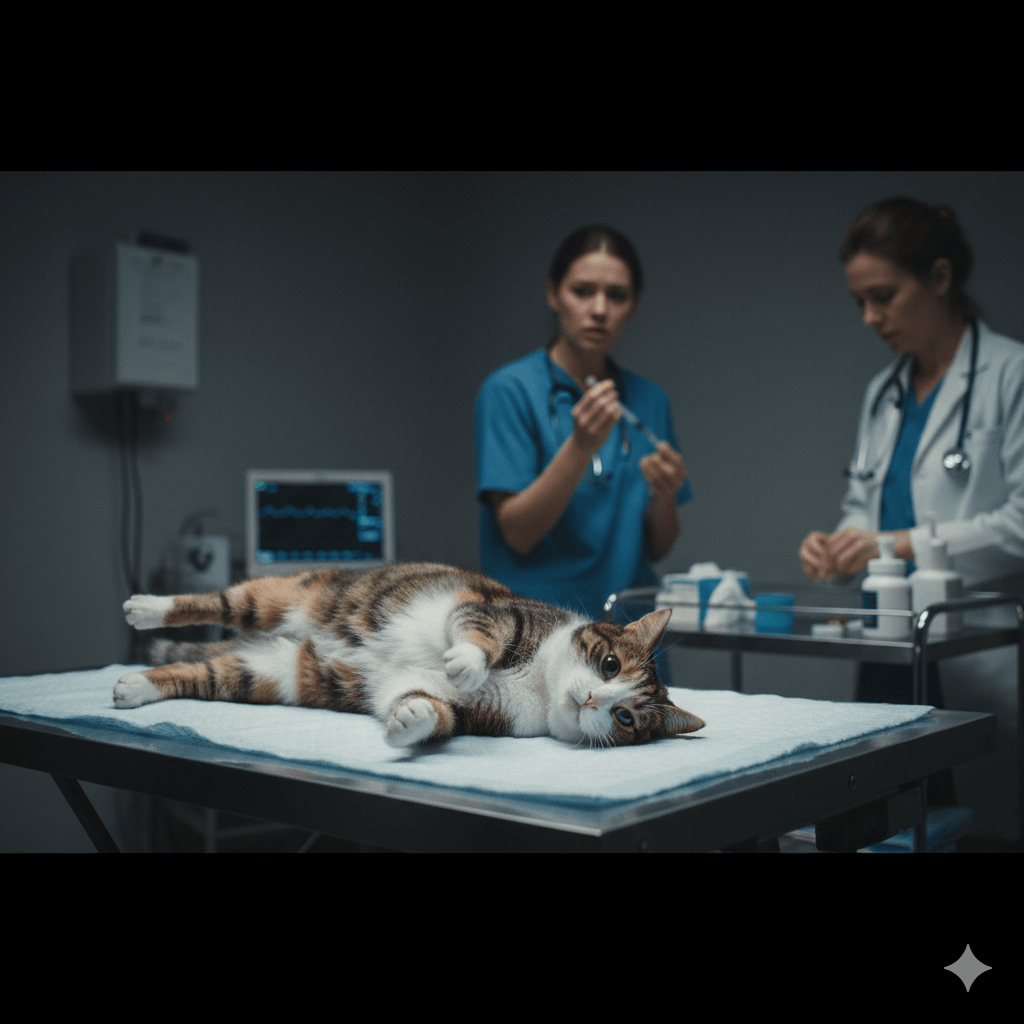
Veterinary Diagnosis and Emergency Treatment
At the clinic, your vet will prioritize stopping the seizure before determining the cause. Rapid intervention protects the brain and supports vital functions.
- IV Anti-Seizure Medications:
Benzodiazepines like diazepam or midazolam are given intravenously to quickly suppress seizure activity. - Supportive Care:
Oxygen therapy, IV fluids, and temperature regulation help stabilize your cat during and after the crisis. - Blood Work and Toxin Screening:
Initial tests assess liver, kidney, glucose, and electrolyte levels to rule out metabolic causes. - Advanced Imaging (If Stable):
MRI or CT scans may be recommended later to evaluate for tumors, inflammation, or structural issues in the brain. - Hospitalization for Monitoring:
Cats often need 24–48 hours of observation to ensure seizures don’t recur and to begin long-term management.
The goal is not just to stop the current episode but to prevent future ones through targeted therapy.
Long-Term Management and Prognosis
After the emergency is controlled, ongoing care focuses on preventing recurrence and addressing the root cause. Many cats live well with proper management.
- Daily Anti-Epileptic Medication:
Drugs like phenobarbital, levetiracetam, or zonisamide may be prescribed long-term to reduce seizure frequency. - Regular Blood Monitoring:
Medication levels and organ function must be checked periodically to ensure safety and effectiveness. - Seizure Diaries:
Track dates, duration, triggers, and behavior changes to help your vet adjust treatment over time. - Environmental Modifications:
Reduce stress, maintain routine, and eliminate access to toxins to lower seizure risk. - Realistic Prognosis Discussions:
Outcomes vary—cats with treatable causes (e.g., toxins) often recover fully, while those with brain tumors may have a guarded outlook.
With consistent care and close veterinary partnership, many cats enjoy months or years of good quality life after an episode.
Special Considerations for Senior Cats and Kittens
Age significantly influences both risk and recovery. Older cats and young kittens need tailored approaches due to physiological vulnerabilities.
- Senior Cats:
More likely to have underlying conditions like kidney disease or brain tumors—seizures may be the first noticeable sign. - Kittens Under 6 Months:
Rarely develop true epilepsy; seizures often point to congenital issues, infections, or severe parasitism. - Slower Drug Metabolism in Elders:
Older cats process medications more slowly, requiring lower doses and closer monitoring for side effects. - Fragility During Seizures:
Both seniors and kittens are at higher risk of injury or aspiration during prolonged episodes due to weaker muscles. - Diagnostic Caution:
Anesthesia for MRI is riskier in very young or old cats, so vets may start with less invasive tests first.
Age isn’t a barrier to care—but it does shape the treatment strategy and long-term expectations.
When to Consider Quality-of-Life Decisions
In some cases—especially with progressive neurological disease—frequent or uncontrolled status epilepticus episodes may impact your cat’s well-being.
- Increasing Medication Side Effects:
Lethargy, loss of coordination, or appetite changes from drugs can reduce daily joy. - Frequent Emergency Visits:
Repeated episodes despite treatment may signal a worsening condition that’s hard to control. - Inability to Engage in Normal Behaviors:
If your cat no longer grooms, plays, or seeks affection, quality of life may be declining. - Veterinary Prognosis Guidance:
Your vet can help assess whether further intervention aligns with your cat’s comfort and dignity. - Compassionate End-of-Life Planning:
When seizures become relentless and unmanageable, humane euthanasia may be the kindest choice.
These decisions are deeply personal—but always rooted in love and your cat’s best interest.
Frequently Asked Questions About Status Epilepticus in Cats
Can a cat survive status epilepticus?
Yes—many cats survive if treated promptly, though outcomes depend on the underlying cause and how quickly care begins.
What should I do if my cat has a seizure at home?
Stay calm, time the episode, keep your cat safe from injury, and call your vet immediately if it lasts over 2 minutes.
Are certain cat breeds more prone to seizures?
No strong breed predisposition exists in cats (unlike some dog breeds), though any cat can develop neurological issues.
Can stress trigger status epilepticus?
While stress may lower the seizure threshold, it rarely causes status epilepticus alone—it usually reveals an existing condition.
Is status epilepticus painful for cats?
Cats are unconscious during the seizure and don’t feel pain then, but the aftermath (disorientation, muscle soreness) can be distressing.
Supporting Your Cat Through Crisis and Recovery
Witnessing your cat in status epilepticus is terrifying—but your presence, advocacy, and swift action are powerful forms of care. Behind the medical interventions lies a deeper truth: your love and attention anchor your cat during their most vulnerable moments. With modern veterinary neurology, many cats not only survive but thrive after such an event, returning to purring, napping, and curling up in your lap as before. Stay informed, partner closely with your vet, and trust your instincts—you know your cat best. And remember: even in the face of neurological storms, the bond you share remains a steady light guiding them home.
How Fast Can a Cat Lose Weight: Best 7 Expert Tips! – Safe rates, warning signs & vet-approved strategies for healthy feline weight loss.
How Fast Can a Dog Lose Weight: Best 7 Expert Tips! – Safe rates, red flags, and vet-approved strategies for healthy dog weight loss.
Understanding Pilar Cyst in Cats: Best 7 Expert Tips! – Spot, assess & care for benign feline skin cysts with vet-backed guidance.
Understanding Pilar Cyst in Dogs: Best 7 Expert Tips! – Identify, monitor & manage benign skin cysts safely with vet-approved guidance.




