Understanding Tracheitis in Cats: Best 7 Expert Tips!
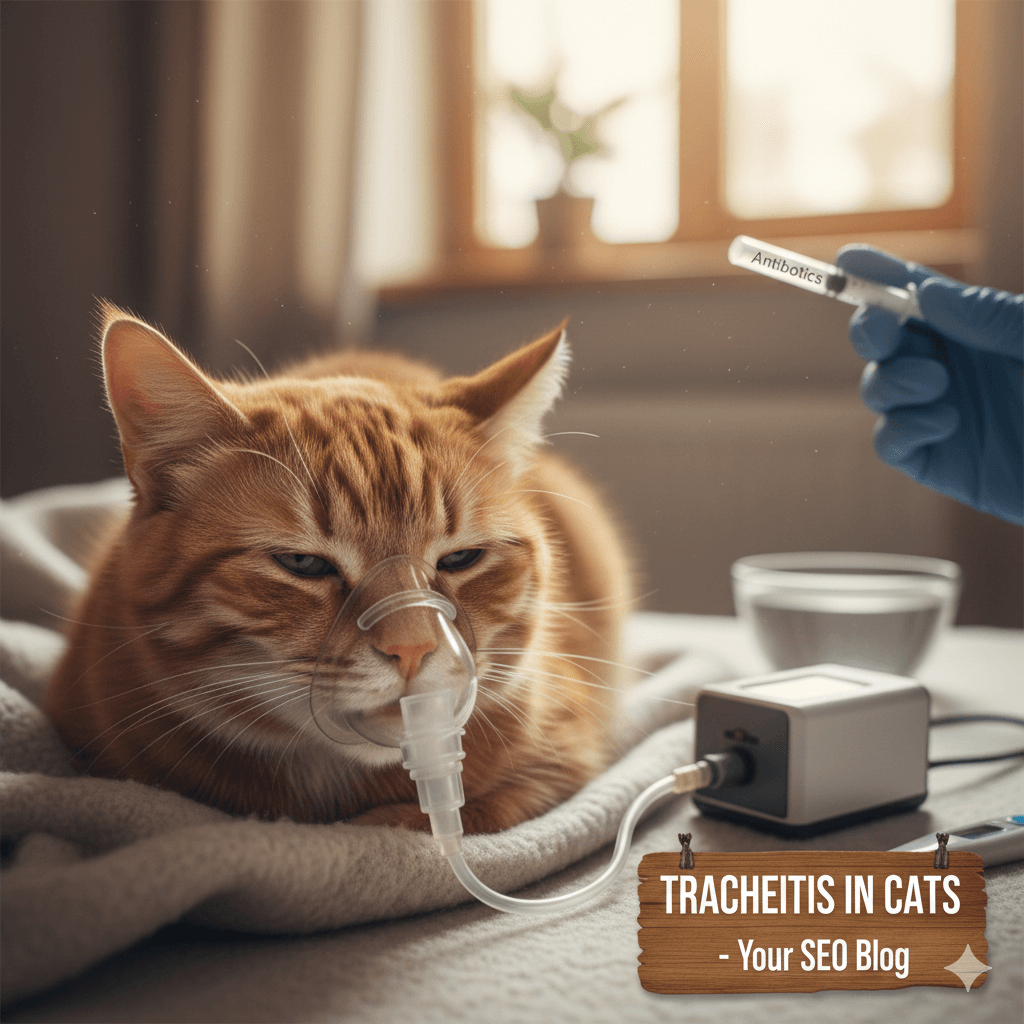
If your cat is coughing persistently, breathing noisily, or showing signs of throat discomfort, tracheitis—an inflammation of the windpipe—could be the cause. Though less common than other feline respiratory issues, tracheal inflammation can range from mild irritation to a serious medical concern. Early recognition and proper care are essential to ease your cat’s distress and prevent complications. While some cases resolve with rest and supportive care, others may signal an underlying infection or chronic condition. Understanding the key signs and triggers helps you act swiftly and support your cat’s recovery with confidence.
Common Signs Your Cat May Have Tracheitis
Tracheitis in cats typically manifests through respiratory and behavioral changes that reflect discomfort in the upper airway. Symptoms often mimic those of a cold or mild asthma, but the location and nature of the inflammation set it apart. Watch for these consistent indicators, especially if they persist beyond a few days:
- Harsh, Dry Cough:
Your cat may produce a loud, hacking cough that sounds like something is stuck in their throat—often worse after excitement or pressure on the neck. - Noisy or Labored Breathing:
Wheezing, rasping, or a high-pitched sound during inhalation (stridor) can occur if the trachea narrows due to swelling. - Gagging or Retching Motions:
Cats may appear to try to clear their throat repeatedly, sometimes mistaken for attempts to vomit a hairball. - Reluctance to Meow or Altered Voice:
Hoarseness, reduced volume, or complete silence may happen if inflammation affects the larynx near the trachea. - Neck Extension While Breathing:
Your cat might stretch their neck forward and open their mouth slightly to ease airflow through a constricted windpipe.
While occasional coughing can be normal, repeated or worsening signs over 2–3 days warrant a veterinary evaluation to rule out serious causes.
When to Worry: Red Flags Beyond Typical Symptoms
Although many cases of tracheal irritation are mild, certain symptoms signal a worsening condition or secondary issue that needs urgent care. Vigilance during the first 48 hours can prevent critical complications like airway obstruction or pneumonia:
- Coughing Up Blood:
Even small streaks of blood suggest significant mucosal damage or ulceration in the trachea or lungs. - Blue or Pale Gums:
A bluish tint (cyanosis) or pale color indicates poor oxygenation—a true emergency requiring immediate intervention. - Open-Mouth Breathing:
Cats are obligate nose breathers; if they breathe through their mouth consistently, their airway is likely compromised. - Lethargy or Collapse:
Severe respiratory distress can lead to exhaustion, weakness, or even fainting due to low oxygen levels. - Swelling or Pain in the Neck Area:
Visible swelling, heat, or your cat flinching when touched near the throat may point to abscesses, trauma, or foreign bodies.
If any of these occur, seek emergency veterinary care without delay—airway issues can escalate rapidly in cats.
Check this guide 👉Lymphosarcoma in Cats: Best 7 Expert Tips!
Check this guide 👉Campylobacter in Cats: Best 7 Expert Tips!
Check this guide 👉Trigeminal Neuritis Symptoms in Cats: Best 7 Expert Tips!
Typical Tracheitis Signs | Emergency Warning Signs |
|---|---|
Occasional dry cough | Coughing with blood or foam |
Mild voice change | Complete loss of meow or stridor |
Brief gagging after collar use | Open-mouth breathing at rest |
Normal energy between episodes | Lethargy or hiding for hours |
Appetite slightly reduced | Refusing food or water entirely |
Causes Behind Feline Tracheitis
Tracheal inflammation in cats rarely occurs in isolation—it’s usually triggered by infectious agents, environmental factors, or physical irritation. Identifying the root cause helps guide both treatment and prevention strategies for long-term respiratory health:
- Viral Infections:
Feline herpesvirus (FHV-1) and calicivirus are leading causes, often part of upper respiratory infections that spread to the trachea. - Bacterial Complications:
Secondary invaders like Bordetella or Mycoplasma can worsen inflammation, especially in stressed or immunocompromised cats. - Inhaled Irritants:
Smoke, strong perfumes, cleaning chemicals, or dust can directly irritate the tracheal lining, triggering coughing and swelling. - Collar Trauma or Pressure:
Pulling on a neck collar—especially during leash walks or sudden jerks—can bruise or inflame the trachea. - Foreign Objects or Growths:
Rarely, inhaled plant material, polyps, or tumors in the throat can mimic or cause tracheal inflammation.
Addressing the underlying trigger is often more effective than treating symptoms alone—especially in recurrent cases.
At-Home Care Strategies for Mild Tracheal Irritation
For mild, non-emergency cases confirmed by your vet, supportive care at home can soothe your cat’s throat and support healing. The goal is to reduce irritation, maintain hydration, and minimize stress on the respiratory system:
- Switch to a Harness:
Immediately stop using neck collars; a soft, well-fitted harness eliminates pressure on the inflamed trachea. - Use a Humidifier:
Adding moisture to dry indoor air (especially in winter) can ease breathing and soothe irritated airways—place it in your cat’s favorite room. - Reduce Environmental Irritants:
Avoid aerosols, scented candles, and strong detergents; opt for fragrance-free, pet-safe cleaning products. - Encourage Hydration:
Offer fresh water, wet food, or low-sodium broth to keep mucous membranes moist and support natural clearance. - Limit Stress and Overexertion:
Keep your cat calm and indoors; avoid loud noises, visitors, or vigorous play until symptoms subside.
With consistent, gentle care, most mild cases improve within 3–5 days—but always follow your vet’s specific instructions.
Preventing Future Episodes of Tracheal Inflammation
Prevention centers on minimizing exposure to known triggers while supporting your cat’s overall immune and respiratory health. Proactive habits can significantly reduce recurrence, especially in multi-cat households or sensitive individuals:
- Keep Vaccinations Updated:
Core vaccines for feline herpesvirus and calicivirus help prevent the most common infectious causes of tracheitis. - Use Harnesses Consistently:
Even for brief outdoor trips or indoor leash training, a harness is always safer than a neck collar. - Maintain Clean Air Quality:
Use HEPA air filters, vacuum regularly, and avoid smoking near your cat to reduce airborne irritants. - Support Immune Health:
Provide balanced nutrition, reduce chronic stress, and consider L-lysine supplements (under vet guidance) for herpesvirus-prone cats. - Isolate New or Sick Cats:
If introducing a new cat or one shows respiratory signs, keep them separated until cleared by a vet to prevent spread.
Long-term prevention isn’t just about avoiding one episode—it’s about creating a healthier, lower-risk environment for your feline companion.
Special Considerations for Kittens, Seniors, and At-Risk Cats
Certain cats face higher risks from tracheitis due to anatomy, immunity, or preexisting conditions. These groups require closer monitoring and often earlier intervention to avoid complications:
- Kittens Under One Year:
Their immune systems are still developing, and their small airways are more easily obstructed by even mild swelling. - Senior Cats:
Age-related decline in lung function or hidden heart disease can worsen the impact of respiratory inflammation. - Brachycephalic Breeds:
Persians, Himalayans, and other flat-faced cats already have compromised airways—tracheitis can tip them into crisis quickly. - Cats with Chronic Herpesvirus:
These individuals may suffer recurrent tracheal flare-ups during stress, requiring lifelong management strategies. - Immunocompromised Cats:
Those with FIV, FeLV, or on immunosuppressive drugs are more prone to severe or prolonged infections.
For these vulnerable cats, even subtle coughing should prompt a vet visit—delaying care can be dangerous.
What to Expect During a Veterinary Visit
If tracheitis is suspected, your vet will perform a comprehensive workup to confirm the diagnosis and rule out emergencies like asthma, heart disease, or foreign bodies. Here’s what typically happens:
- Thorough Physical Exam:
The vet will listen to your cat’s lungs and trachea, check gum color, and gently palpate the neck for swelling or pain. - Diagnostic Imaging:
X-rays or fluoroscopy may be used to visualize tracheal narrowing, collapse, or signs of pneumonia. - Viral or Bacterial Testing:
PCR swabs from the mouth or throat can identify herpesvirus, calicivirus, or bacterial pathogens. - Airway Endoscopy (if needed):
In persistent cases, a tiny camera may be inserted to directly view the trachea for ulcers, polyps, or strictures. - Personalized Treatment Plan:
This may include anti-inflammatories, antibiotics, antivirals, nebulization, or cough suppressants—never given without professional guidance.
A clear diagnosis ensures your cat receives the right care, not just symptom masking—and gives you peace of mind during recovery.
Frequently Asked Questions About Tracheitis in Cats
Can tracheitis in cats go away on its own?
Mild cases caused by temporary irritation may resolve in a few days, but infectious or chronic forms usually require treatment to prevent worsening.
Is tracheitis contagious to other cats?
Yes—if caused by viruses like herpes or calicivirus, it can spread through saliva, sneezing, or shared bowls, especially in multi-cat homes.
Can a collar really cause tracheitis?
Absolutely. Repeated tugging or tight collars can bruise or inflame the trachea—switching to a harness is a critical first step in treatment.
How is tracheitis different from feline asthma?
Asthma causes wheezing and difficulty exhaling due to lower airway constriction, while tracheitis typically causes a dry, hacking cough and noisy inhalation.
Should I give my cat cough medicine?
Never use human cough syrups—they often contain toxic ingredients like acetaminophen. Only use medications prescribed by your veterinarian.
Supporting Your Cat Through Recovery and Beyond
Seeing your cat struggle to breathe or cough repeatedly can be deeply unsettling—but with timely care and a calm, supportive environment, most cats recover fully from tracheitis. Your role goes beyond medication: it’s in the quiet presence, the clean air, the gentle switch to a harness, and the patience during healing. Use this experience to strengthen your cat’s long-term health through vaccination, stress reduction, and attentive observation. Because every breath your cat takes without strain is a testament to your love and vigilance—and that’s the greatest gift you can give your feline friend.
Newfoundland Dog Personality: Best 7 Expert Tips! – Discover the gentle, loyal, and protective nature of this giant breed perfect for families.
Can Hot Pavement Burn Your Cats Paws? Best 7 Expert Tips! – Learn how to protect your cat’s paws from hot surfaces and prevent painful burns this summer.
Can Hot Pavement Burn Your Dogs Paws? Best 7 Expert Tips! – Learn how to protect your dog’s paws from hot surfaces and ensure safe summer walks.
Irish Wolfhound Size: Best 7 Expert Tips! – Discover the ideal height, weight, and care tips for this majestic giant breed. Learn how to manage their impressive stature responsibly.