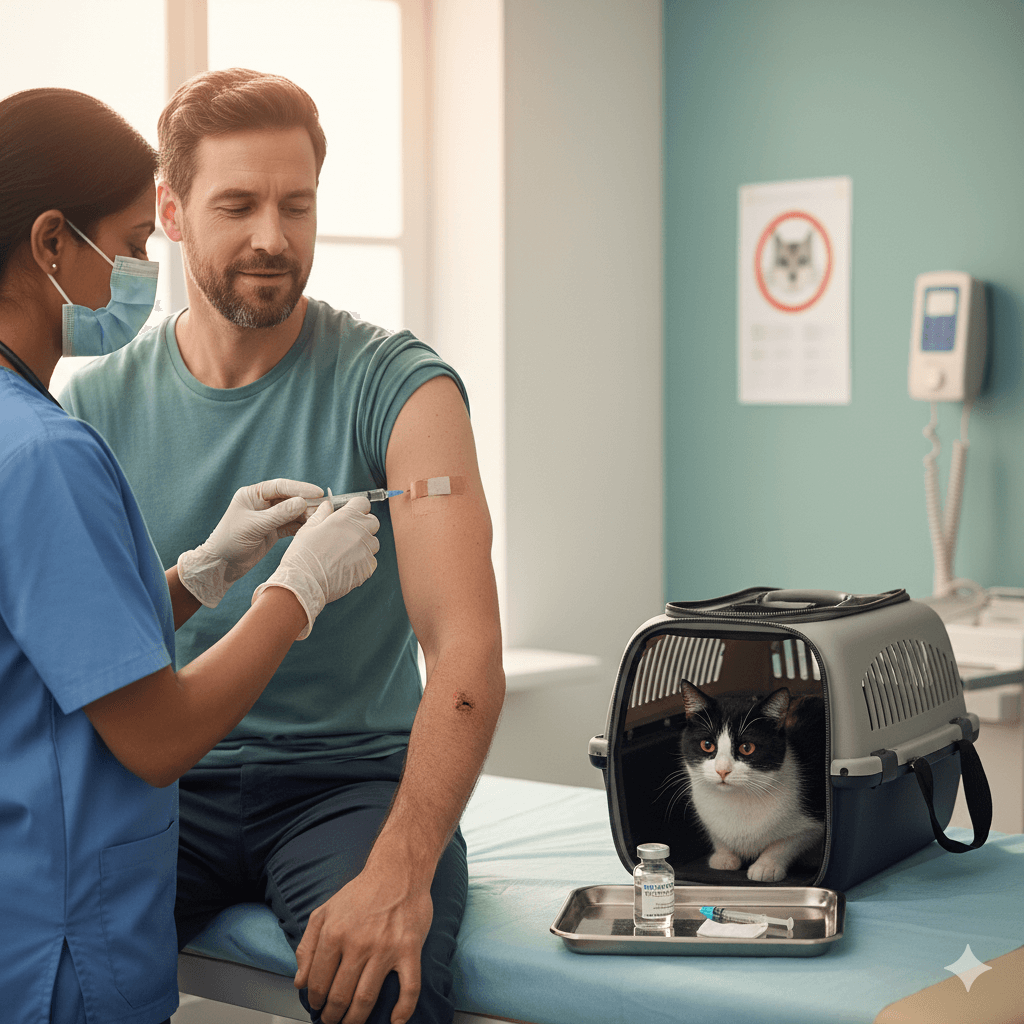
Understanding Tetanus Shot After Cat Bite
A cat bite may seem minor, but it can pose hidden risks—including tetanus, a serious bacterial infection that affects the nervous system. While cats don’t carry the tetanus bacterium themselves, the bacteria Clostridium tetani live in soil, dust, and manure and can enter your body through even a small puncture wound. Knowing whether you need a tetanus shot after a cat bite depends on your vaccination history, the bite’s severity, and how quickly you clean and treat the wound. Prompt attention can prevent complications and ensure peace of mind during recovery.
How Cat Bites Can Lead to Tetanus Risk
Cat bites create deep puncture wounds that seal quickly, trapping bacteria inside and creating an ideal environment for infection—including tetanus. Though rare, tetanus is preventable with up-to-date vaccinations, making awareness crucial after any skin-breaking injury:
- Deep Puncture Wounds:
Cats’ sharp teeth inject bacteria deep into tissue, and the small entry point often closes fast, hiding contamination beneath the skin. - Environmental Exposure:
If the bite occurs outdoors or the cat’s claws/mouth contacted soil or dirt, Clostridium tetani spores may have been introduced into the wound. - Delayed Wound Care:
Waiting hours to clean the bite increases infection risk, including tetanus, especially if your last booster was years ago. - Rusty Objects Not Required:
Contrary to myth, tetanus doesn’t require contact with rust—any contaminated wound, including animal bites, can be a gateway. - Higher Risk for Unvaccinated Individuals:
If you haven’t had a tetanus shot in over 10 years (or never completed the primary series), your protection may be insufficient.
While tetanus from cat bites is uncommon, the consequences are severe—making prevention through vaccination and wound care essential.
Signs You Might Need a Tetanus Shot After a Cat Bite
Not every cat bite requires a tetanus booster, but certain factors signal it’s time to consult a healthcare provider. Your vaccination status and wound characteristics guide this decision:
- Last Tetanus Shot Over 5 Years Ago (for dirty wounds):
Deep or contaminated bites are considered “dirty wounds”; if your last booster was more than 5 years ago, a shot is typically recommended. - Uncertain or Incomplete Vaccination History:
If you don’t remember your last tetanus shot or never finished the childhood series, assume you’re not protected. - Visible Dirt or Debris in the Wound:
Soil, fur, or saliva trapped in the puncture increases bacterial load and tetanus risk. - Delayed Medical Attention:
Bites treated more than 6–8 hours later carry higher infection potential, warranting prophylactic measures. - Compromised Immune System:
Conditions like diabetes, HIV, or immunosuppressive therapies weaken your body’s ability to fight off spores.
When in doubt, err on the side of caution—tetanus is nearly 100% preventable with timely vaccination.
Check this guide 👉Understanding If a Cat Bite Is Dangerous: Best 7 Expert Tips
Check this guide 👉My Cat Bites Me and Holds On: Best 7 Expert Tips!
Check this guide 👉Cat Bite vs Dog Bite: Best 7 Expert Tips!
When a Tetanus Shot Is Likely Needed | When It’s Usually Not Required |
|---|---|
Bite breaks the skin and last booster was >5 years ago | Superficial scratch with no bleeding and up-to-date vaccines |
Wound is deep, dirty, or contaminated | Minor bite cleaned immediately and last shot within 5 years |
Unknown or incomplete vaccine history | Fully vaccinated within the past 2–3 years |
Bite occurred outdoors or in unsanitary conditions | Indoor-only cat, clean bite, no debris |
Signs of infection (redness, swelling, pus) | No skin breakage—just bruising or pressure marks |
Immediate First Aid Steps After a Cat Bite
Proper wound care in the first hour can drastically reduce infection risk, including tetanus. Act quickly and methodically to protect your health:
- Wash Thoroughly with Soap and Water:
Rinse under running water for 3–5 minutes, using mild soap to flush out bacteria from deep tissue channels. - Apply Antiseptic Solution:
Use hydrogen peroxide, iodine, or chlorhexidine to disinfect the area after cleaning—avoid alcohol, which can damage tissue. - Control Bleeding Gently:
Apply light pressure with a clean cloth; slight bleeding actually helps expel contaminants. - Cover with a Sterile Bandage:
Once clean and dry, protect the wound from further contamination with a breathable dressing. - Monitor for Early Infection Signs:
Redness, warmth, swelling, or pain within 24 hours may signal bacterial infection requiring antibiotics.
Never ignore a cat bite—even small wounds can escalate rapidly without proper care.
When to Seek Medical Attention After a Cat Bite
While many bites heal at home, certain red flags mean professional evaluation is non-negotiable. Cat bites carry a high risk of Pasteurella and other infections, making timely care critical:
- Deep or Bleeding Wounds That Won’t Stop:
Persistent bleeding or wounds deeper than 1–2 mm may need sutures or drainage. - Signs of Infection Within 24–48 Hours:
Increasing pain, red streaks, pus, fever, or swollen lymph nodes indicate advancing infection. - Bite on Hand, Face, or Joint:
These areas are prone to severe complications due to dense nerve and tendon networks. - Immunocompromised Status:
Those with weakened immune systems face higher risks of systemic infection. - Uncertainty About Rabies Exposure:
If the cat is stray, feral, or unvaccinated, rabies prophylaxis may also be considered alongside tetanus.
A healthcare provider can assess your tetanus risk, clean the wound professionally, and prescribe antibiotics if needed.
Understanding Tetanus: How It Develops and Why It’s Dangerous
Tetanus isn’t contagious—it’s caused by a toxin released by Clostridium tetani bacteria in oxygen-poor environments like deep wounds. Once activated, the toxin attacks nerves, causing muscle rigidity and spasms that can be life-threatening:
- Incubation Period Varies:
Symptoms typically appear 3–21 days after exposure, though it can take up to several months. - Early Signs Include Jaw Stiffness:
“Lockjaw” (trismus) is a classic first symptom, followed by neck stiffness, difficulty swallowing, and abdominal rigidity. - Severe Cases Cause Respiratory Failure:
Muscle spasms can interfere with breathing, requiring intensive care and ventilator support. - No Cure—Only Supportive Treatment:
Once tetanus develops, treatment focuses on managing symptoms while the body recovers, often over weeks or months. - High Fatality Rate Without Vaccination:
Up to 10–20% of tetanus cases are fatal, even with modern care—highlighting why prevention is vital.
Thankfully, the tetanus vaccine is highly effective and widely available, making this disease almost entirely avoidable.
Tetanus Vaccination Guidelines for Adults and Children
Keeping your tetanus shots up to date is the single best defense after any wound, including cat bites. The CDC outlines clear recommendations based on age and risk:
- Primary Series in Childhood:
Children receive DTaP (diphtheria, tetanus, pertussis) at 2, 4, 6, 15–18 months, and 4–6 years. - Booster at Age 11–12:
Tdap (tetanus, diphtheria, acellular pertussis) is given once in adolescence. - Adult Boosters Every 10 Years:
Td (tetanus and diphtheria) or Tdap every decade maintains immunity; Tdap is preferred once for pertussis coverage. - Post-Injury Boosters:
For dirty wounds, a booster is advised if the last shot was over 5 years ago—regardless of age. - Pregnant Women Should Get Tdap:
Recommended during each pregnancy (27–36 weeks) to protect newborns from whooping cough and maintain maternal immunity.
If you’re unsure about your status, check your immunization records—or ask your doctor for a titer test or precautionary booster.
Special Considerations for High-Risk Individuals
Certain groups face elevated dangers from tetanus and should act swiftly after any cat bite, even seemingly minor ones. Extra vigilance can be life-saving:
- Elderly Adults Over 65:
Immune response weakens with age, and vaccine protection may wane faster—booster adherence is critical. - People with Chronic Wounds or Diabetes:
Poor circulation and slower healing increase susceptibility to deep infections. - Outdoor Workers or Gardeners:
Frequent soil exposure means higher baseline spore contact—cat bites in these settings are higher risk. - Travelers to Developing Regions:
In areas with limited medical access, ensuring tetanus immunity before travel is a must. - Those with Wound Contamination from Manure or Rusty Objects:
Though not from the cat itself, environmental co-exposure multiplies risk significantly.
For these individuals, a cat bite isn’t just a scratch—it’s a potential medical event requiring prompt evaluation.
Frequently Asked Questions About Tetanus Shot After Cat Bite
Do I really need a tetanus shot after a cat bite?
It depends: if your last booster was over 5 years ago and the bite broke the skin, yes—especially if the wound is deep or dirty.
Can tetanus develop from a clean indoor cat bite?
It’s unlikely but not impossible. If the wound is superficial and you’re up to date on vaccines, risk is very low.
How soon after a bite should I get a tetanus shot?
Ideally within 48 hours—though getting it even 5–7 days later can still offer protection during the incubation period.
Is the tetanus shot safe?
Yes. Side effects are usually mild (sore arm, slight fever) and far less dangerous than tetanus itself.
What if I can’t remember my last tetanus shot?
Assume you’re not protected. Getting an extra booster is safe and far better than risking infection.
Protecting Yourself Beyond the Bite
A cat bite can be a wake-up call about both wound care and vaccination habits. While most heal without issue, the potential for serious infections like tetanus means proactive steps matter. By keeping your tetanus immunizations current, cleaning bites immediately, and seeking care when needed, you turn a moment of pain into a lesson in preparedness. Remember, your immune system can only fight what it’s trained to recognize—so stay up to date, stay informed, and never underestimate the power of prevention. In the end, a small shot today can spare you a far greater ordeal tomorrow.
How to Check Your Cat for a Fever: Best 7 Expert Tips! – Learn the signs, safe temperature checks, and when to see a vet. Keep your feline healthy and happy!
How to Check Your Dog for a Fever: Best 7 Expert Tips! – Learn the signs, safe temperature checks, and when to see a vet if your dog has a fever.
Hypothyroidism and Its Impact on Cat Skin: Best 7 Tips! – Discover how hypothyroidism affects your cat’s skin, spot symptoms early, and learn effective care strategies to keep your feline healthy.
Hypothyroidism and Its Impact on Dog Skin: Best 7 Tips! – Discover how hypothyroidism affects your dog’s skin, spot symptoms early, and learn effective care strategies to restore their health.




