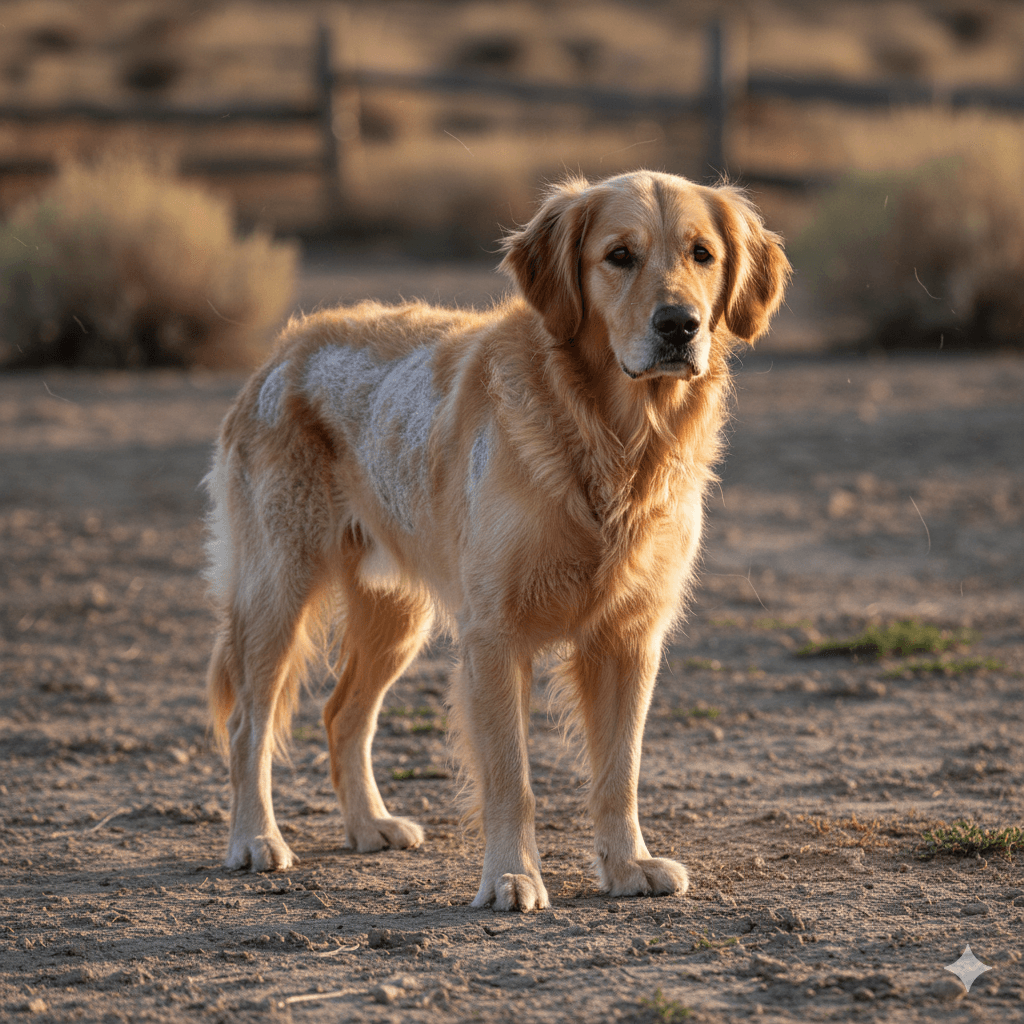
Understanding Sebaceous Adenitis in Dogs: Best 7 Expert Tips!
Sebaceous adenitis is a rare but serious inflammatory skin condition that affects dogs of all breeds—though some are more predisposed than others. It targets the sebaceous glands, which produce oils essential for healthy skin and coat, leading to dryness, scaling, hair loss, and secondary infections. While not life-threatening on its own, sebaceous adenitis significantly impacts your dog’s comfort and quality of life if left unmanaged. Early detection, consistent treatment, and lifelong care are key to keeping your pup comfortable and thriving. With expert guidance and devoted care, many dogs live full, happy lives despite this chronic condition.
What Is Sebaceous Adenitis and How Does It Develop?
Sebaceous adenitis (SA) is an autoimmune or inherited disorder in which a dog’s immune system mistakenly attacks and destroys its own sebaceous (oil-producing) glands. Without these glands, the skin becomes dry, flaky, and prone to infection. The exact cause isn’t fully understood, but genetics, immune dysfunction, and breed predisposition play major roles.
- Autoimmune Origin:
In many cases, the body’s immune system attacks healthy sebaceous glands, mistaking them for foreign invaders—triggering chronic inflammation. - Genetic Predisposition:
Certain breeds like Standard Poodles, Akitas, Samoyeds, and Vizslas show higher incidence rates, suggesting a hereditary component. - Onset Timing:
Symptoms often appear between 1–5 years of age, though cases in puppies and older dogs have been documented. - Progressive Nature:
SA typically worsens over time if untreated, spreading from localized patches to larger areas of the body. - Misdiagnosis Risk:
Because early signs mimic allergies, fungal infections, or poor grooming, SA is frequently overlooked until advanced.
Accurate diagnosis by a veterinary dermatologist—often via skin biopsy—is essential to distinguish SA from other skin conditions and start proper management.
Common Signs and Symptoms to Watch For
Recognizing the early warning signs of sebaceous adenitis can make a huge difference in your dog’s long-term outcome. Symptoms vary by coat type but generally follow a consistent pattern of dryness, scaling, and hair loss.
- Dry, Scaly Skin:
Large white or gray flakes appear, especially along the back, head, and ears—often mistaken for dandruff. - Patchy Hair Loss:
Alopecia begins in circular or irregular patches, with hair becoming brittle and falling out easily. - Dull or Brittle Coat:
The fur loses its natural sheen and softness, feeling coarse or straw-like to the touch. - Secondary Skin Infections:
Without protective oils, bacteria or yeast can invade, causing odor, redness, pustules, or itching. - Breed-Specific Presentations:
In long-coated breeds (e.g., Poodles), mats and silvery scales cling to hair shafts; in short-coated dogs (e.g., Vizslas), skin looks moth-eaten or “moth-wing” textured.
If you notice these signs—especially in a high-risk breed—schedule a veterinary dermatology consult promptly.
Check this guide 👉Understanding Addisons Disease in Dogs: Best 7 Expert Tips!
Check this guide 👉Understanding Pemphigus in Dogs: Best 7 Expert Tips!
Check this guide 👉Understanding Pododermatitis in Dogs: Best 7 Expert Tips!
Early Warning Signs | Advanced or Complicated Signs |
|---|---|
Mild flaking on the back | Widespread hair loss across trunk and tail |
Slight dullness in coat | Thickened, wrinkled, or hyperpigmented skin |
Occasional scratching | Foul odor from bacterial yeast overgrowth |
Small bald patches near ears | Open sores or crusting from chronic inflammation |
No response to allergy treatments | Lethargy or discomfort due to chronic skin pain |
Diagnosis: How Vets Confirm Sebaceous Adenitis
Because SA mimics many other dermatological issues, diagnosis requires more than just a visual exam. Your vet will rule out common causes before pursuing definitive testing.
- Physical and Coat Examination:
The vet assesses distribution of hair loss, scale type, and skin texture—clues that suggest SA over allergies or parasites. - Skin Scrapings and Cytology:
These rule out mange, fungal infections (like ringworm), and bacterial overgrowth as primary causes. - Fungal and Bacterial Cultures:
Used if secondary infection is suspected to guide antibiotic or antifungal therapy. - Skin Biopsy (Gold Standard):
A small skin sample is sent to a lab; histopathology showing absent or inflamed sebaceous glands confirms SA. - Response to Trial Therapy:
Sometimes vets initiate SA treatment empirically—if your dog improves significantly, it supports the diagnosis.
A biopsy remains the only definitive way to diagnose sebaceous adenitis, so don’t hesitate to ask for a referral to a veterinary dermatologist if needed.
Treatment and Management Strategies for Lifelong Care
There is no cure for sebaceous adenitis—but with consistent, tailored care, most dogs achieve good symptom control and comfort. Treatment focuses on replacing lost oils, reducing inflammation, and preventing infections.
- Medicated Shampoos and Rinses:
Keratolytic shampoos (with salicylic acid or benzoyl peroxide) remove scales; emollient rinses (with propylene glycol or oils) restore moisture. - Topical Oil Replacements:
Many owners apply diluted baby oil, mineral oil, or specialized sprays to mimic natural sebum—left on for 1–2 hours before bathing off. - Oral Fatty Acid Supplements:
Omega-3 and omega-6 supplements support skin barrier function and reduce inflammation over time. - Immunomodulatory Medications:
In severe cases, vets may prescribe cyclosporine or corticosteroids to suppress the autoimmune response. - Antibiotics or Antifungals (As Needed):
Used short-term to treat secondary infections that worsen discomfort and delay healing.
Consistency is crucial—most dogs require weekly or biweekly bathing routines for life, along with daily skin monitoring.
Breeds Most at Risk and Genetic Considerations
While any dog can develop sebaceous adenitis, certain breeds carry a much higher genetic risk. Responsible breeding and early screening can help reduce prevalence.
- Standard Poodles:
The most commonly affected breed; many experts recommend screening before breeding. - Akitas:
Often develop a more severe, systemic form that includes weight loss and fever in addition to skin signs. - Samoyeds:
Typically show symptoms before age 3, with rapid progression if untreated. - Vizslas:
Present with subtle, short-coat symptoms that are easily missed until widespread. - Havanese, Springer Spaniels, and Lhasa Apsos:
Also reported with increased frequency, though less commonly than the top three.
If you own or plan to adopt one of these breeds, discuss SA screening with your breeder and vet—even if your dog looks healthy.
Home Care Tips for Daily Comfort and Prevention
Managing sebaceous adenitis at home requires dedication, but your efforts directly impact your dog’s comfort and skin health. Small daily habits make a big difference.
- Stick to a Bathing Schedule:
Most SA dogs need medicated baths every 1–2 weeks—use vet-recommended products and avoid human shampoos. - Gentle Brushing:
Daily brushing removes loose hair and scales, prevents matting, and stimulates blood flow to the skin. - Humidify Dry Environments:
Low humidity worsens dry skin; consider a pet-safe humidifier during winter months. - Avoid Harsh Grooming Tools:
Use soft brushes or rubber grooming gloves—never slicker brushes that can irritate fragile skin. - Monitor for Infection Signs:
Check weekly for redness, odor, or oozing—early treatment prevents painful flare-ups.
Your hands-on care is the cornerstone of your dog’s SA management plan—and your bond often grows stronger through this shared routine.
When to See a Veterinary Dermatologist
While general vets can manage mild cases, complex or progressive sebaceous adenitis benefits from specialist care. A veterinary dermatologist offers advanced diagnostics and tailored protocols.
- No Improvement After 4–6 Weeks of Home Care:
If scales and hair loss persist despite routine treatment, a specialist can adjust your plan. - Recurrent Skin Infections:
Frequent antibiotics suggest poor disease control—time for a deeper evaluation. - Breed Known for Severe SA (e.g., Akita):
Proactive specialist involvement can prevent systemic complications. - Uncertain Diagnosis:
If your vet suspects SA but hasn’t confirmed it, a dermatologist can perform precise biopsies and interpretation. - Need for Long-Term Medication Guidance:
Drugs like cyclosporine require careful dosing and monitoring best handled by a skin specialist.
Early referral often leads to better long-term outcomes and fewer emergency visits down the road.
Frequently Asked Questions About Sebaceous Adenitis in Dogs
Is sebaceous adenitis contagious to other dogs or humans?
No—it’s an autoimmune or genetic condition, not an infection, so it cannot spread to people or pets.
Can sebaceous adenitis be cured?
Unfortunately, no. It’s a chronic condition requiring lifelong management, but many dogs live comfortably with proper care.
Does diet affect sebaceous adenitis?
While diet doesn’t cause SA, high-quality food with added omega fatty acids supports overall skin health and may improve outcomes.
How often should I bathe my dog with SA?
Most dogs need medicated baths every 1–2 weeks, but your vet will tailor the frequency based on severity and coat type.
Should I avoid breeding a dog with sebaceous adenitis?
Yes. Because SA has a strong genetic link, affected dogs—and often their close relatives—should not be bred to prevent passing it on.
Supporting Your Dog Through a Chronic Skin Journey
A sebaceous adenitis diagnosis can feel overwhelming at first—but with knowledge, consistency, and love, your dog can still enjoy a joyful, comfortable life. This condition isn’t just about skin deep; it’s a testament to your commitment as a caregiver. Every bath, every brush, every vet visit is an act of devotion that your dog feels deeply. While the road may be lifelong, you’re not alone: with the right team and routine, you can transform a challenging diagnosis into a story of resilience and care. After all, your dog doesn’t see their dry patches or missing fur—they see you, their safe place, their unwavering source of comfort. And that makes all the difference.
Understanding Cat Storm Anxiety: Best 7 Expert Tips! – Calm your cat’s fear of thunder with vet-approved strategies and a safe space.
Understanding Dog Storm Anxiety: Best 7 Expert Tips! – Calm your dog’s storm fear with proven strategies, expert advice, and long-term solutions.
Understanding Carolina Dog Temperament: Best 7 Expert Tips! – Discover expert insights on loyalty, training & care for this rare American primitive breed.
Understanding Euthyroid Sick Syndrome in Cats: Best 7 Tips! – Learn how illness affects thyroid tests & avoid misdiagnosis in your cat.