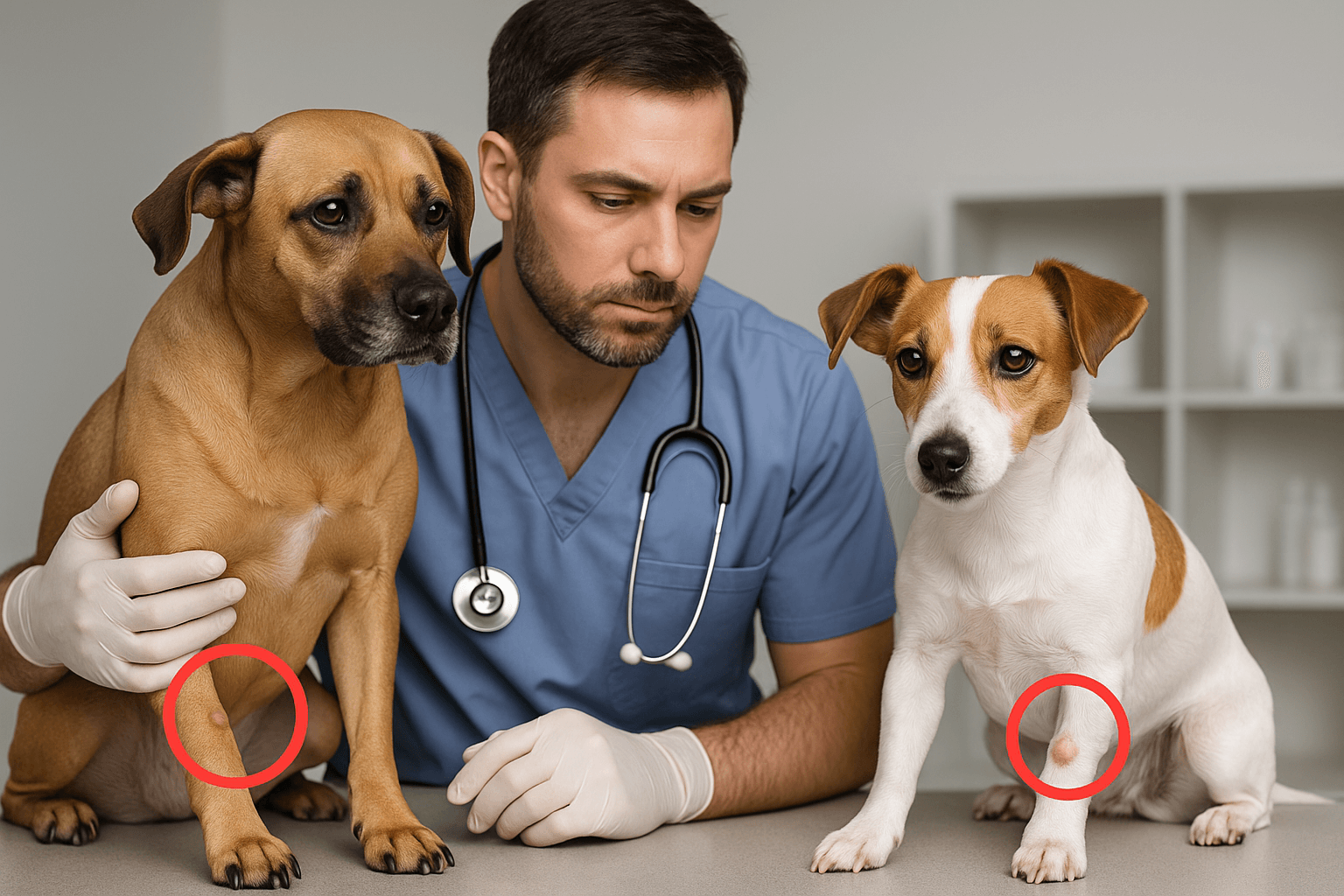
Mast Cell Tumor vs Histiocytoma in Dogs: Understanding Two Common Skin Growths
When you spot a lump on your dog’s skin, it’s natural to feel a surge of worry. Not all bumps are cause for alarm—but knowing the difference between common growths like mast cell tumors and histiocytomas can make all the difference in your pup’s care. These two skin conditions appear similar at first glance, yet they differ significantly in origin, behavior, and treatment. While one often resolves on its own, the other may require urgent medical attention. This guide walks you through what every dog owner should know to respond wisely—and quickly—when a mystery bump shows up.
Origins and Biological Nature of Mast Cell Tumors
Mast cell tumors (MCTs) arise from mast cells, a type of white blood cell involved in the immune system’s allergic and inflammatory responses. These tumors are among the most common skin cancers in dogs and can vary widely in appearance and aggression.
- Immune System Origin:
Mast cells normally help defend against parasites and regulate inflammation, but genetic mutations can cause them to multiply uncontrollably. - Variable Malignancy:
MCTs are graded from I to III—low-grade tumors may be benign and localized, while high-grade ones can spread rapidly to lymph nodes, spleen, or bone marrow. - Breed Predisposition:
Breeds like Boxers, Boston Terriers, Bulldogs, and Golden Retrievers are at higher risk, though any dog can develop an MCT. - Age Factor:
Most commonly diagnosed in middle-aged to older dogs (average age 8–9 years), though younger dogs aren’t immune. - Internal Potential:
While often skin-based, MCTs can also form internally in the spleen, liver, or gastrointestinal tract—making early detection critical.
Although invisible to the naked eye, the biology of mast cell tumors demands serious attention, as their behavior can shift from harmless to life-threatening with little warning.

Origins and Biological Nature of Histiocytomas
Histiocytomas are benign skin tumors that originate from Langerhans cells—specialized immune cells in the skin that help detect foreign invaders. Unlike mast cell tumors, these growths are typically harmless and often disappear without treatment.
- Immune Surveillance Role:
Langerhans cells act as “sentinels” in the epidermis; histiocytomas form when these cells proliferate abnormally but non-cancerously. - Self-Resolving Nature:
Most histiocytomas regress spontaneously within 2–3 months as the dog’s immune system recognizes and eliminates them. - Common in Young Dogs:
They primarily affect dogs under 3 years old, especially breeds like Dachshunds, Cocker Spaniels, and Boxers. - Single Lesion Pattern:
Histiocytomas usually appear as one smooth, round, hairless bump—often on the head, ears, or limbs. - No Metastasis Risk:
These tumors do not spread to other organs and pose no systemic threat, even if left untreated.
This self-limiting quality makes histiocytoma one of the few skin growths that veterinarians may choose to monitor rather than remove immediately.
Check this guide 👉Types of Dog Tumors: Best 7 Expert Tips!
Check this guide 👉Low-Grade Mast Cell Tumors in Dogs: Best 7 Expert Tips!
Check this guide 👉Vascular Tumors in Dogs: Best 7 Expert Tips!
| Mast Cell Tumor Traits | Histiocytoma Traits |
|---|---|
| Can be malignant and metastasize | Always benign, never spreads |
| Often irregular, inflamed, or changing in size | Smooth, firm, dome-shaped, and consistent |
| Common in older dogs (8+ years) | Mostly in young dogs (<3 years) |
| May cause systemic symptoms (vomiting, lethargy) | No systemic effects; purely cosmetic |
| Requires biopsy, grading, and often surgery | Often monitored; may resolve without intervention |
Clinical Appearance and Common Locations
While both mast cell tumors and histiocytomas present as skin lumps, their visual and tactile differences can offer early clues to their identity—though a veterinary diagnosis is always essential.
- Mast Cell Tumor Appearance:
MCTs can look like anything: a wart, a soft mass, an ulcerated sore, or even a fluctuating bump that swells and shrinks due to histamine release. - Histiocytoma Appearance:
Typically appears as a small (1–2 cm), shiny, hairless, red or pink nodule with a smooth surface—often described as “button-like.” - MCT Preferred Sites:
Frequently found on the trunk, limbs, and especially the groin or perineal area, though they can appear anywhere. - Histiocytoma Preferred Sites:
Most common on the head, ears, neck, and front legs—areas with thinner skin and more immune activity. - Behavior on Touch:
MCTs may feel soft or firm and can become itchy or inflamed when scratched; histiocytomas are usually non-itchy and painless.
Despite appearances, visual inspection alone isn’t enough—what looks like a harmless bump could be a high-grade mast cell tumor in disguise.
Diagnostic Approaches and Testing
Accurate diagnosis is the cornerstone of appropriate treatment. Fortunately, veterinarians have reliable tools to distinguish between these two conditions quickly.
- Fine Needle Aspirate (FNA):
A quick, minimally invasive test where cells are extracted with a thin needle and examined under a microscope—often conclusive for both MCT and histiocytoma. - Cytology Clues for MCT:
Mast cells contain distinctive purple granules that are easily identifiable under staining, confirming the diagnosis. - Cytology Clues for Histiocytoma:
Shows uniform, round histiocytes with clear cytoplasm and indented nuclei—classic “fried egg” appearance. - Biopsy for Uncertainty:
If FNA is inconclusive or the tumor appears aggressive, a full biopsy with histopathology provides grading and margin assessment. - Additional Staging (for MCT):
If mast cell tumor is confirmed, bloodwork, lymph node aspirates, and abdominal ultrasound may be needed to check for spread.
Early and accurate diagnosis prevents unnecessary surgery for histiocytomas—and ensures timely, life-saving intervention for malignant mast cell tumors.
Treatment Strategies and Prognosis
Treatment paths diverge dramatically based on the diagnosis, reflecting the fundamental difference between a benign growth and a potential cancer.
- Mast Cell Tumor Treatment:
Surgery is the gold standard; wide margins are crucial. Radiation or chemotherapy may follow for high-grade or incomplete removals. - Histiocytoma Management:
Often no treatment is needed. If the lump is bothersome or doesn’t regress by 3 months, simple surgical removal suffices. - Prognosis for Low-Grade MCT:
With complete surgical excision, Grade I tumors often carry an excellent long-term prognosis. - Prognosis for High-Grade MCT:
Grade III tumors or those with metastasis have a guarded outlook, though newer targeted therapies (like tyrosine kinase inhibitors) offer hope. - Histiocytoma Outcome:
Resolution is expected in 6–12 weeks; recurrence is rare, and no long-term effects occur.
Choosing the right path hinges entirely on the correct diagnosis—underscoring why no skin lump should be ignored.
Behavioral and Systemic Warning Signs
While histiocytomas remain localized and silent, mast cell tumors can trigger body-wide reactions due to histamine and cytokine release.
- Darier’s Sign (MCT Only):
Rubbing the tumor may cause it to swell or redden temporarily—a unique reaction caused by mast cell degranulation. - Gastrointestinal Symptoms:
Dogs with MCT may vomit, have diarrhea, or lose appetite due to excess histamine irritating the stomach lining. - Lethargy or Collapse:
In severe cases, systemic histamine release can lead to low blood pressure or shock—medical emergencies. - Histiocytoma Behavior:
The dog acts completely normal—no pain, itching, or systemic changes—unless the lump is traumatized. - Owner Observation Tips:
Track changes in size, texture, and your dog’s overall behavior; photos and notes help veterinarians assess progression.
Your dog’s behavior is a powerful diagnostic clue—listen to what their body is telling you.
Prevention, Monitoring, and When to See a Vet
While neither condition is fully preventable, vigilant monitoring can catch issues early and improve outcomes significantly.
- Weekly Skin Checks:
Gently run your hands over your dog’s body weekly to detect new lumps early—especially in at-risk breeds. - Photograph New Growths:
Take dated photos to track size or color changes over days or weeks. - Never Assume “It’s Just a Cyst”:
Even small, slow-growing lumps warrant veterinary evaluation—mast cell tumors can masquerade as harmless bumps. - Seek Immediate Care for:
Rapid growth, ulceration, bleeding, or behavioral changes like vomiting or lethargy. - Post-Diagnosis Follow-Up:
Dogs with a history of MCT need lifelong skin surveillance, as recurrence or new tumors are possible.
Proactive care turns uncertainty into control—and early action into better outcomes.
Frequently Asked Questions About Mast Cell Tumor vs Histiocytoma in Dogs
Can a histiocytoma turn into cancer?
No. Histiocytomas are always benign and do not transform into malignant tumors. They either regress or are easily removed.
Are mast cell tumors painful for dogs?
Not usually in early stages, but they can become itchy, inflamed, or painful if ulcerated or infected. Systemic effects may cause discomfort.
How long does it take to get FNA results?
Many vets can examine the sample in-house within minutes. If sent to a lab, results typically return in 1–3 days.
Can diet help manage mast cell tumors?
While no diet cures MCT, low-histamine diets and omega-3 fatty acids may support overall immune balance during treatment—consult your vet first.
Should I remove a histiocytoma if it’s not bothering my dog?
Generally no—unless it’s in a high-friction area (like a paw) or hasn’t regressed after 3 months. Observation is often the best approach.
When in Doubt, Get It Checked Out
Finding a lump on your dog’s skin doesn’t have to mean panic—but it should always mean a visit to the vet. Mast cell tumors and histiocytomas may look alike to the untrained eye, but their implications couldn’t be more different. One is a manageable, often fleeting quirk of a young dog’s immune system; the other is a serious condition that demands swift, informed action. By understanding these differences, you empower yourself to advocate for your dog’s health with clarity and confidence. After all, your vigilance—and that quick trip to the clinic—could be the key to peace of mind or even a life saved.
Pemphigus Erythematosus in Cats: Best 7 Expert Tips! – Learn to recognize symptoms, manage flare-ups, and improve your cat’s quality of life.
Pemphigus Erythematosus in Dogs: Best 7 Expert Tips! – Discover causes, symptoms, and treatment options to manage this autoimmune skin condition effectively.
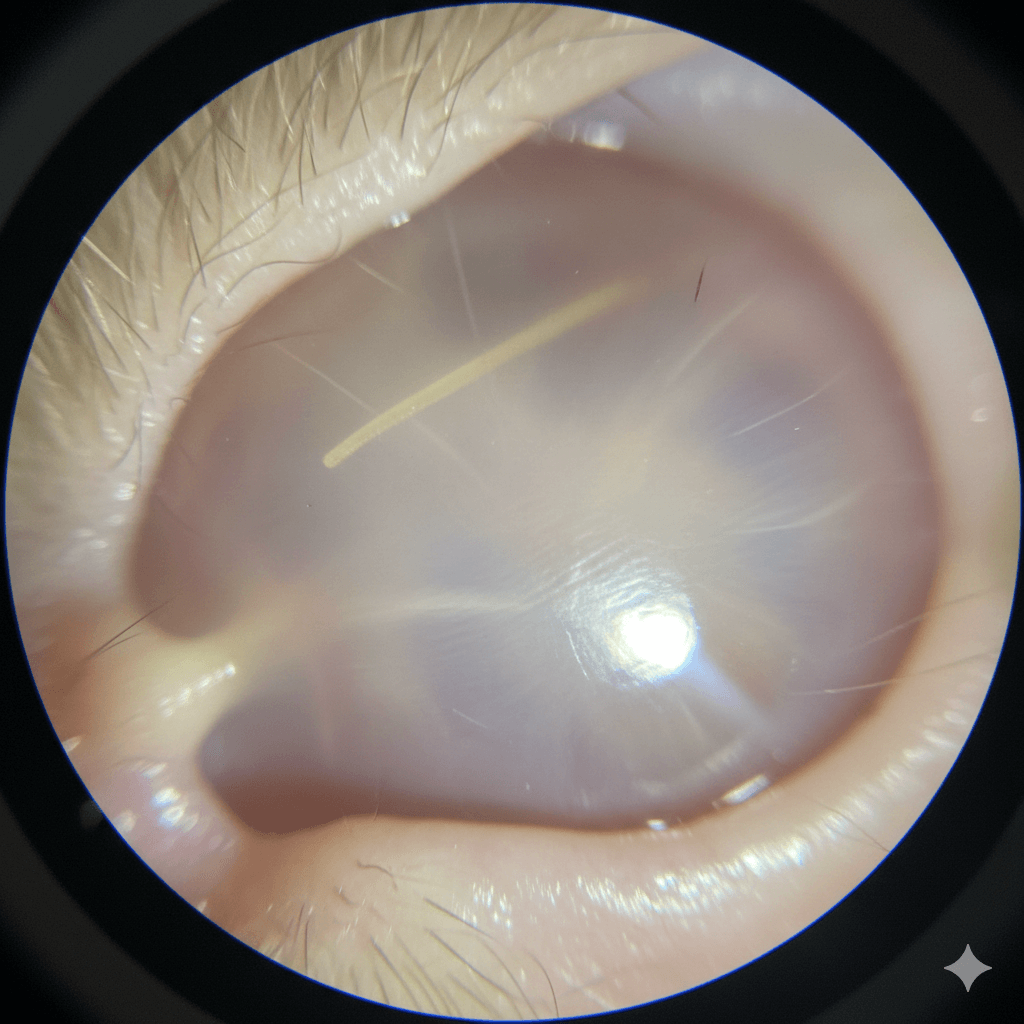
Cat Tympanic Membrane: Best 7 Expert Tips! – Learn how to protect your cat’s eardrum, spot issues early, and ensure lifelong auditory health.
Dog Tympanic Membrane: Best 7 Expert Tips! – Learn how to protect your dog’s eardrum, spot issues early, and ensure lifelong ear health with expert advice.