Understanding Everted Laryngeal Saccules in Dogs
If your dog struggles to breathe, especially during excitement or exercise, it could be more than just “normal snoring”—it might be a sign of everted laryngeal saccules. This condition, often linked to brachycephalic airway syndrome, occurs when soft tissues in the voice box are sucked into the airway, worsening breathing difficulties. While it may start subtly, it can progress to serious respiratory distress if ignored. Early recognition and veterinary evaluation are essential to restore your dog’s comfort and prevent complications. With proper care, many dogs go on to live full, active lives—even with this delicate airway issue.
What Are Everted Laryngeal Saccules?
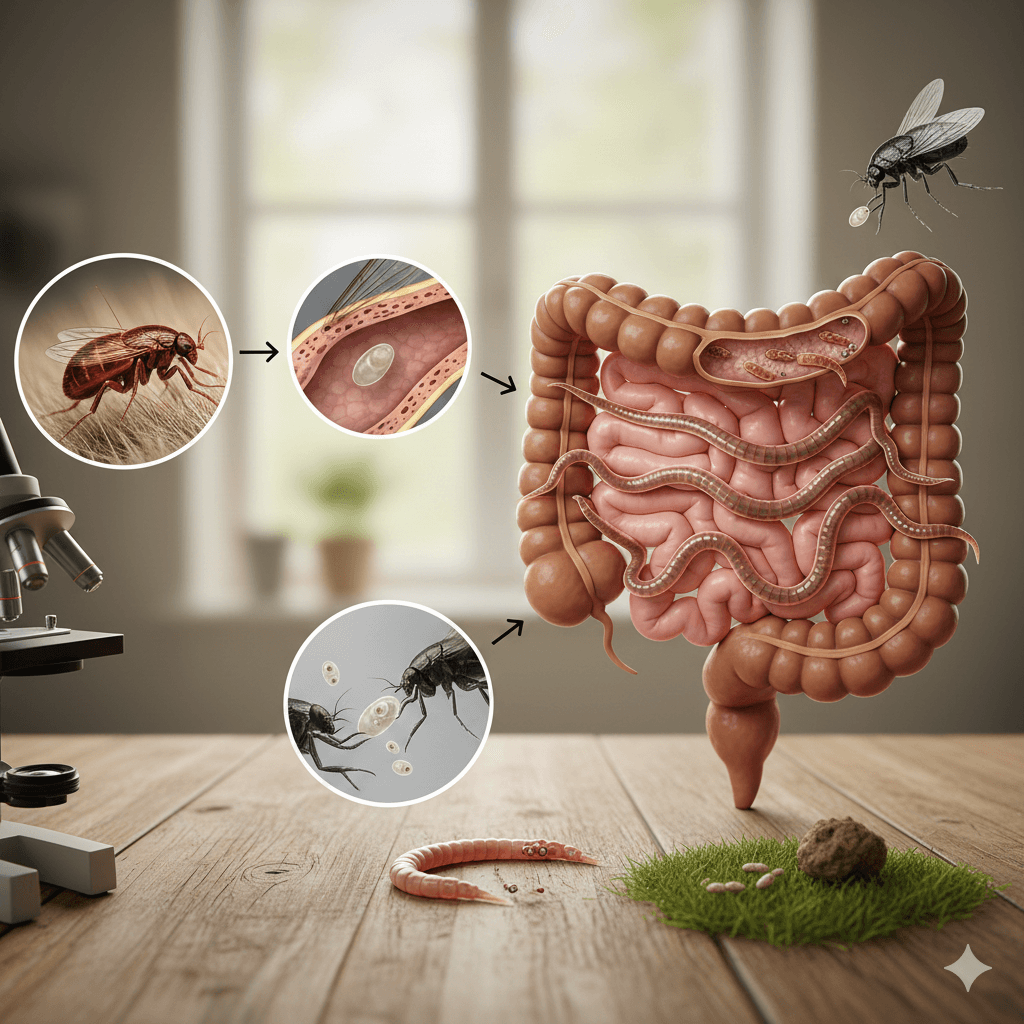
Everted laryngeal saccules are small pouches located just inside the larynx (voice box) that normally sit recessed. In affected dogs, chronic airway resistance—often from narrowed nostrils or an elongated soft palate—creates negative pressure that pulls these saccules outward into the airway. This further obstructs airflow and can create a dangerous cycle of worsening breathing. Understanding their role helps clarify why early intervention matters:
- Anatomical Location:
The laryngeal saccules are paired mucosal pouches near the vocal folds, meant to protect and lubricate the larynx—not block airflow. - Mechanism of Eversion:
Persistent labored breathing generates suction that flips the saccules inside out, like turning a sock inside out, dragging them into the tracheal opening. - Progressive Nature:
Once everted, they worsen obstruction, leading to louder breathing, fatigue, and even collapse during heat or stress. - Commonly Secondary:
This condition rarely appears alone—it’s typically part of brachycephalic obstructive airway syndrome (BOAS) in short-nosed breeds. - Visible Only Internally:
Diagnosis requires sedation and laryngeal examination by a vet; you can’t see everted saccules from the outside.
Left untreated, everted saccules can escalate from a mild breathing quirk to a life-threatening emergency—making awareness a vital part of responsible ownership.
Breeds Most at Risk for This Condition
While any dog can develop airway issues, everted laryngeal saccules overwhelmingly affect brachycephalic (flat-faced) breeds due to their compressed skull anatomy. These dogs are born with structural airway limitations that predispose them to chronic breathing strain:
- English Bulldog:
Their extremely shortened muzzle and narrow nostrils create high resistance, making them one of the highest-risk breeds. - French Bulldog:
Despite their small size, Frenchies often suffer from multiple BOAS components, including everted saccules by middle age. - Pug:
Compact airways and a tendency toward obesity amplify breathing effort, accelerating saccule eversion. - Boston Terrier:
Known for expressive eyes and a square head, they also inherit narrowed nasal passages that strain the larynx over time. - Shih Tzu and Pekingese:
Though slightly less extreme than bulldogs, these toy breeds still face elevated risk due to flattened faces and soft palate issues.
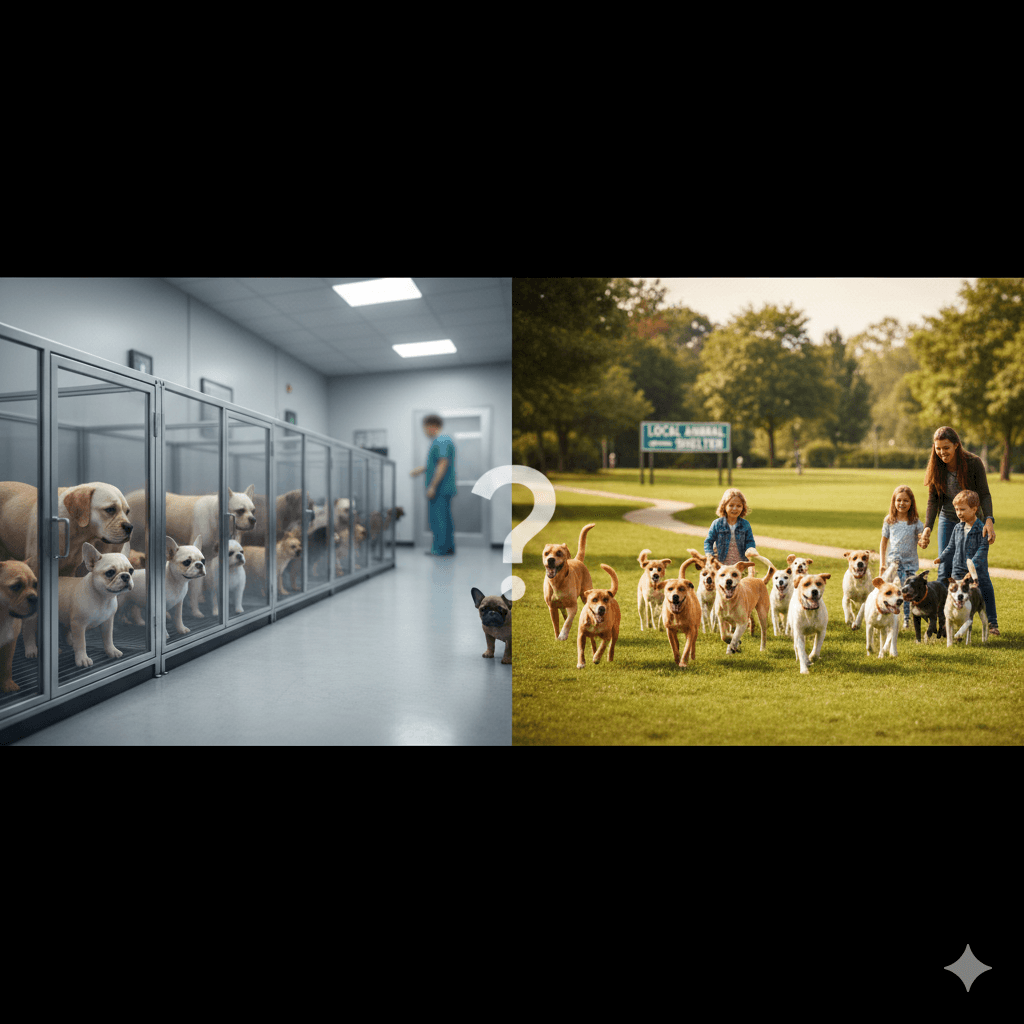
If you own or are considering one of these breeds, proactive airway assessment—even in seemingly healthy dogs—can catch problems before they escalate.
Check this guide 👉French Bulldog Health Issues: Best 7 Expert Tips!
Check this guide 👉Greater Swiss Mountain Dog Health Issues: Best 7 Tips!
Check this guide 👉Healthiest Dog Breeds: Best 7 Expert Tips!
Early Warning Signs | Advanced or Emergency Indicators |
|---|---|
Noisy breathing (stertor or stridor) | Blue-tinged gums or tongue (cyanosis) |
Exercise intolerance | Collapse after mild activity or heat exposure |
Gagging or retching without vomiting | Open-mouth breathing even at rest |
Snoring louder than usual | Severe anxiety or panic during breathing episodes |
Coughing after excitement | Inability to lie down comfortably |
Diagnostic Process: How Vets Confirm the Condition
Because everted laryngeal saccules aren’t visible externally, diagnosis requires a hands-on, internal evaluation under controlled conditions. Your vet will use specific methods to confirm the issue and assess its severity:
- Physical Exam and History Review:
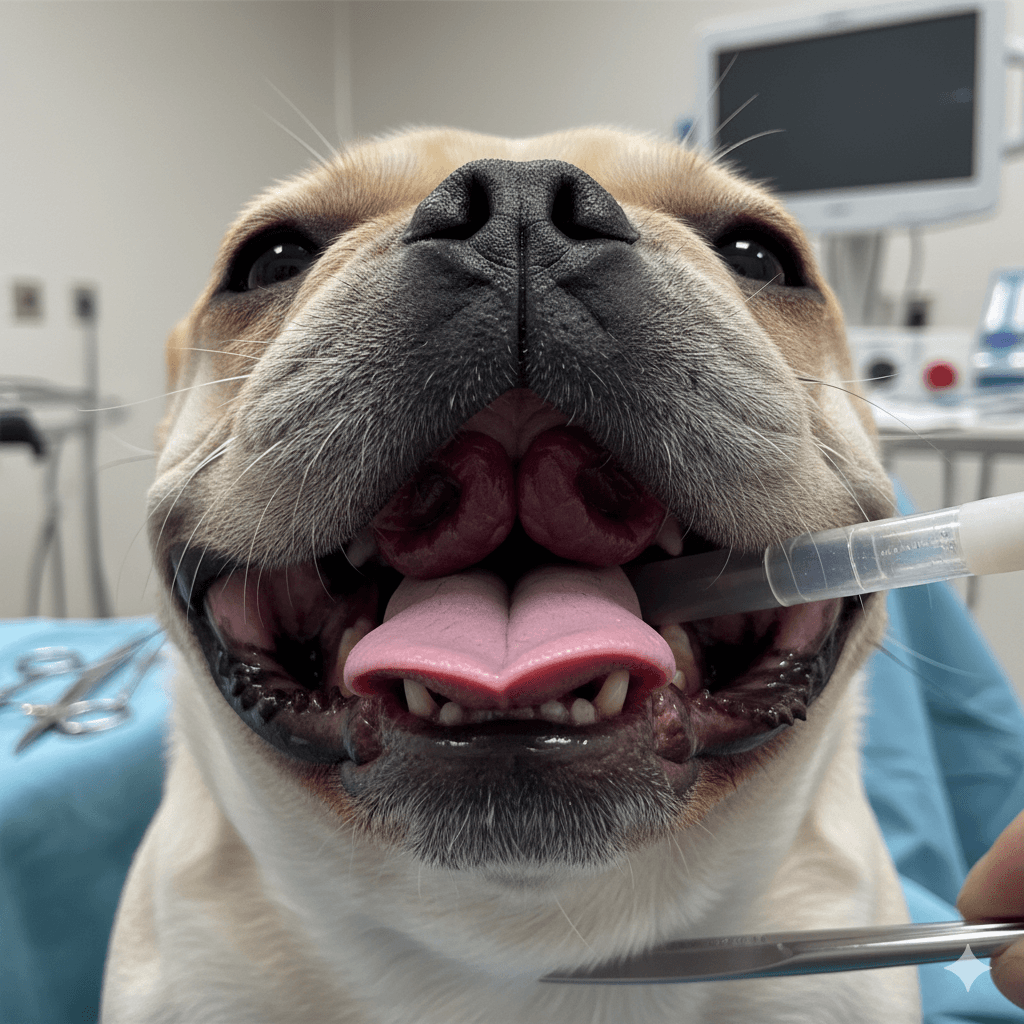
Your vet will ask about breathing patterns, activity tolerance, and breed history to assess BOAS likelihood. - Sedated Laryngeal Examination:
Light sedation allows safe visualization of the larynx using a laryngoscope to check if saccules are protruding into the airway. - Chest X-rays:
These help rule out heart disease, pneumonia, or tracheal collapse that could mimic or complicate the condition. - BOAS Grading System:
Many specialists use standardized airflow tests or functional grading to determine surgical need and prognosis. - Referral to a Specialist:
In complex cases, a veterinary surgeon or internal medicine specialist may lead diagnostics for precision.
Accurate diagnosis is the foundation for effective treatment—and can prevent unnecessary emergency visits down the line.
Treatment Options and Surgical Intervention
Once diagnosed, treatment depends on severity—but surgery is often the most effective long-term solution. The goal is to restore unobstructed airflow and break the cycle of progressive airway collapse:
- Sacculectomy (Saccule Removal):
The primary treatment involves surgically trimming the everted tissue using scissors, laser, or electrocautery under general anesthesia. - Combined BOAS Procedures:
Sacculectomy is frequently paired with soft palate shortening and nostril widening (rhinoplasty) for comprehensive airway relief. - Post-Op Intensive Care:
Dogs are closely monitored for swelling, which can temporarily worsen breathing—a few may need temporary intubation. - Medication Support:
Anti-inflammatories, sedatives, or oxygen therapy may be used short-term to support recovery. - Non-Surgical Management (Mild Cases Only):
Weight loss, avoiding heat, and using harnesses (not collars) can help—but won’t reverse eversion once it’s occurred.
Surgery often leads to dramatic improvement in breathing, energy, and quality of life—especially when performed before secondary changes set in.
Preventive Care and Long-Term Management
While you can’t change your dog’s anatomy, you can significantly reduce strain on their airway and delay or avoid complications. Prevention focuses on minimizing triggers and supporting overall respiratory health:
- Maintain Ideal Weight:
Even slight excess weight dramatically increases breathing effort—keep your dog lean through diet and gentle exercise. - Use a Harness, Not a Collar:
Neck pressure from collars compresses the trachea; a well-fitted harness eliminates this risk during walks. - Avoid Heat and Humidity:
Brachycephalic dogs overheat quickly; limit outdoor time on hot days and never leave them in cars. - Schedule Early Airway Screening:
Consider a BOAS evaluation at 6–12 months of age, even if symptoms seem mild—early surgery yields better outcomes. - Provide Calm, Cool Indoor Spaces:
Stress and excitement trigger breathing spikes; create quiet retreats where your dog can relax undisturbed.
Prevention isn’t about perfection—it’s about consistent, thoughtful choices that add up to easier breathing every single day.
What to Expect During Recovery After Surgery
Post-operative care is critical to ensure smooth healing and avoid complications like swelling or infection. Most dogs recover well with attentive home support:
- Hospital Stay (12–24 Hours):
Your dog will likely stay overnight for oxygen support and monitoring as anesthesia wears off. - Restricted Activity for 2 Weeks:
No running, jumping, or rough play—leash walks only, and keep them calm indoors to reduce breathing strain. - Soft Food for a Few Days:
Swallowing may be sore; offer moistened kibble or bland boiled food to ease eating. - Watch for Breathing Changes:
Mild noise is normal initially, but sudden worsening, coughing blood, or distress requires immediate vet contact. - Follow-Up Appointments:
Your vet will check healing at 1–2 weeks and may assess long-term airflow improvement.
Most owners report a “night-and-day” difference in their dog’s breathing, energy, and happiness within a few weeks of surgery.
Potential Complications and When to Seek Emergency Care
Even with treatment, airway conditions carry risks—especially during recovery or in advanced cases. Knowing danger signs can save your dog’s life:
- Acute Airway Obstruction:
Sudden inability to breathe, panic, or collapse is a true emergency—seek veterinary help immediately. - Post-Surgical Swelling:
Some swelling is expected, but excessive swelling can block the airway—watch closely for 48 hours post-op. - Aspiration Pneumonia:
If saccules or palate issues impair swallowing, food or saliva may enter the lungs, causing cough, fever, or lethargy. - Chronic Hypoxia Effects:
Long-term low oxygen can strain the heart—regular cardiac checks may be recommended in severe cases. - Recurrence or Progression:
In rare cases, other tissues (like the laryngeal cartilages) may collapse later, requiring further intervention.
Trust your instincts—if your dog seems “off” or is struggling to catch their breath, don’t wait.
Frequently Asked Questions About Everted Laryngeal Saccules in Dogs
Can everted laryngeal saccules go away on their own?
No—once everted, the tissue won’t return to its normal position without surgical correction.
Is this condition painful for dogs?
Not directly painful, but the constant struggle to breathe causes stress, anxiety, and fatigue.
At what age do dogs typically develop this issue?
Signs often appear between 1–4 years, though earlier in severely affected breeds like English Bulldogs.
Can my dog live a normal life after surgery?
Yes—most dogs experience significant improvement in breathing, stamina, and overall quality of life.
Are there non-surgical alternatives for older dogs?
For high-risk seniors, management focuses on weight control, environmental adjustments, and medications—but surgery remains the only cure.
Giving Your Dog the Gift of Easier Breathing
Watching your dog gasp for air is one of the most helpless feelings a pet owner can face—but the good news is that everted laryngeal saccules are treatable, often with remarkable results. With early detection, skilled veterinary care, and your loving support, your dog can breathe easier, play longer, and enjoy life without constant respiratory strain. Remember, every gentle walk, cool room, and well-fitted harness is an act of care that honors their unique needs. In the end, helping your brachycephalic companion breathe freely isn’t just medicine—it’s love in action, one calm, quiet breath at a time.
Dog Tapeworm Life Cycle: Best 7 Expert Tips! – Learn how tapeworms infect dogs, spot symptoms, and break the cycle with expert prevention strategies.
Anxious Cat Body Language: Best 7 Expert Tips! – Learn to spot signs of stress, understand triggers, and help your cat feel safe and relaxed.
Anxious Dog Body Language: Best 7 Expert Tips! – Learn to spot signs of anxiety, respond effectively, and help your dog feel safe and secure.
Is Breeding Dogs Bad? Best 7 Expert Tips! – Explore the ethics, benefits, and risks of dog breeding to make informed decisions for a better future.