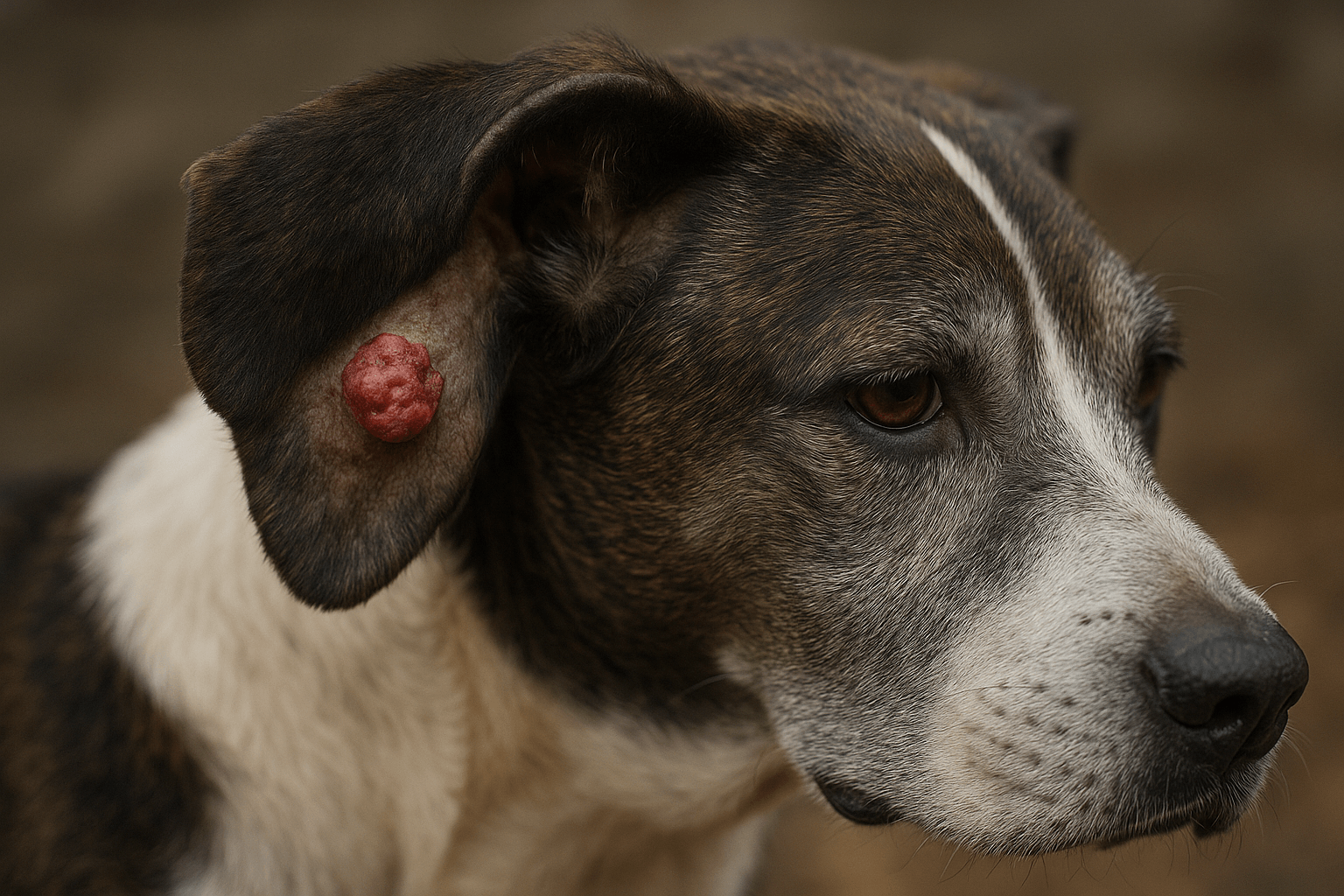
Mast Cell Tumor on a Dogs Ear Flap: What Every Pet Parent Needs to Know
Discovering a bump on your dog’s ear flap can be unsettling—especially when it turns out to be a mast cell tumor, one of the most common skin cancers in canines. These tumors can appear harmless at first, yet their behavior ranges from benign to aggressive, making early recognition critical. The ear flap’s thin skin and rich blood supply create unique challenges for diagnosis and treatment. Understanding your options, from biopsy to surgery, empowers you to act swiftly and confidently. This guide breaks down everything you need to know—without the overwhelm—so you can focus on your dog’s well-being.
What Is a Mast Cell Tumor?
Mast cell tumors (MCTs) arise from mast cells—immune cells involved in allergic responses and inflammation. While they can develop anywhere, the ear flap is a notable location due to its delicate tissue and visibility.
- Unpredictable Behavior:
MCTs vary widely in appearance and aggression; some grow slowly, while others change size daily due to histamine release. - Common in Certain Breeds:
Boxers, Boston Terriers, Bulldogs, and Golden Retrievers have higher predisposition, though any dog can be affected. - Often Misidentified:
Because they can mimic benign cysts or insect bites, MCTs are sometimes dismissed until they grow or ulcerate. - Grading Determines Risk:
Pathologists classify MCTs as Grade I (low risk), II (intermediate), or III (highly aggressive)—guiding treatment decisions. - Ear Flap Vulnerability:
The ear’s thin cartilage and limited tissue margin make surgical removal more complex than on thicker skin areas.
Recognizing that not all lumps are equal—and that location matters—helps ensure timely, appropriate care.

Warning Signs to Watch For
Early detection improves outcomes dramatically. Learn the subtle and obvious clues that a bump on your dog’s ear might be more than just a harmless growth.
- Rapid Size Changes:
MCTs may swell after being touched or fluctuate throughout the day due to histamine release. - Redness or Ulceration:
The surface may become raw, bleed, or crust over, especially if your dog scratches or shakes its head. - Itching or Discomfort:
Your dog might paw at the ear, tilt its head, or show sensitivity when the area is handled. - Multiple Lumps Nearby:
Satellite nodules around the main mass can signal local spread—common in higher-grade tumors. - Swollen Lymph Nodes:
Enlarged lymph nodes near the ear may indicate the tumor is progressing beyond the original site.
If you notice any of these signs, schedule a vet visit right away—don’t wait to “see what happens.”
Check this guide 👉High Grade Mast Cell Tumor Dog: Best 7 Expert Tips!
Check this guide 👉The Costs of Dog Tumor Removal: Best 7 Expert Tips!
Check this guide 👉Mast Cell Tumor vs Histiocytoma in Dogs: Best 7 Expert Tips!
| Benign-Looking Signs | Red Flags for MCT |
|---|---|
| Small, firm, non-painful lump | Lump that changes size daily |
| No redness or discharge | Ulceration or bleeding |
| Stable for weeks | Rapid growth in days |
| Dog ignores the area | Frequent scratching or head shaking |
| Single isolated bump | Multiple nearby nodules |
Diagnostic Steps Your Vet Will Take
Accurate diagnosis is essential before deciding on treatment. Fortunately, veterinarians have reliable tools to assess ear flap masses quickly.
- Fine Needle Aspirate (FNA):
A quick, minimally invasive test where cells are extracted with a needle and examined under a microscope—often done during the initial visit. - Biopsy for Grading:
If FNA suggests MCT, a tissue sample is sent to a lab to determine the tumor grade and guide treatment planning. - Imaging (Ultrasound or CT):
Used to check for spread to lymph nodes, internal organs, or deeper ear structures—especially for Grade II or III tumors. - Bloodwork and Urinalysis:
Help assess overall organ function and detect systemic effects of mast cell disease, like elevated histamine levels. - Staging the Disease:
Based on all results, your vet assigns a clinical stage (I–IV), which predicts prognosis and shapes the treatment roadmap.
These steps ensure your dog gets a precise diagnosis—not guesses—so therapy can be tailored effectively.
Treatment Options for Ear Flap MCTs
Treatment depends on tumor grade, location, size, and whether it has spread. The ear flap’s anatomy influences surgical feasibility and alternatives.
- Surgical Removal:
The gold standard for localized MCTs—but ear flaps offer limited tissue, sometimes requiring specialized techniques or partial ear amputation. - Radiation Therapy:
Excellent for tumors that can’t be fully removed due to ear anatomy; highly effective for local control with minimal side effects. - Chemotherapy or Targeted Drugs:
Used for high-grade, metastatic, or recurrent MCTs; newer drugs like toceranib (Palladia) target mast cell pathways specifically. - Steroid Therapy:
Prednisone may shrink some MCTs temporarily and reduce inflammation, but it’s not a cure—often used alongside other treatments. - Monitoring Low-Grade Tumors:
In rare cases, small Grade I tumors may be watched if surgery poses high risk—but this requires close vet supervision.
A veterinary oncologist can help weigh these options based on your dog’s unique situation and quality-of-life goals.
Why Ear Flap Location Complicates Treatment
The ear flap (pinna) isn’t just skin—it’s thin cartilage with minimal underlying tissue, making MCT management uniquely challenging.
- Limited Surgical Margins:
To ensure clean removal, vets need 1–2 cm of healthy tissue around the tumor—hard to achieve on a narrow ear flap without disfigurement. - Risk of Poor Wound Healing:
The ear’s blood supply and constant motion (from head shaking) increase the chance of complications like dehiscence or infection. - Cosmetic and Functional Concerns:
Large excisions may alter ear shape or lead to scarring that affects airflow or comfort. - Higher Recurrence Risk:
Incomplete removal due to anatomical constraints can allow tumor cells to regrow at the same site. - Need for Specialist Care:
Board-certified surgeons or oncologists often achieve better outcomes with reconstructive techniques or multimodal therapy.
Understanding these limitations helps set realistic expectations and explore all available options.
Post-Treatment Care and Monitoring
Recovery doesn’t end with surgery or therapy—ongoing vigilance is key to catching recurrence early and supporting healing.
- Wound Management:
Keep the ear clean, dry, and protected; use an E-collar to prevent scratching or rubbing during healing. - Medication Compliance:
If your dog is on pain relievers, antihistamines, or targeted drugs, administer exactly as prescribed—don’t skip doses. - Follow-Up Appointments:
Regular check-ups (e.g., every 3 months) with physical exams and possibly repeat imaging help monitor for new growths. - Watch for New Lumps:
Dogs with one MCT have a higher risk of developing others—check your dog’s skin weekly from nose to tail. - Supportive Nutrition:
Antioxidant-rich diets or vet-approved supplements may support immune function during recovery (always consult your vet first).
Consistent aftercare turns treatment success into long-term wellness.
Prevention and Risk Reduction Strategies
While mast cell tumors can’t always be prevented, proactive steps may reduce risk or catch issues early in susceptible dogs.
- Regular Skin Checks:
Perform monthly full-body exams—especially on ears, paws, and belly—where MCTs commonly appear. - Genetic Awareness:
If you own a high-risk breed, discuss screening protocols with your vet even before symptoms arise. - Avoid Chronic Inflammation:
Minimize skin irritants, allergies, or repeated trauma that may theoretically contribute to abnormal cell growth. - Spay/Neuter Timing (Emerging Research):
Some studies suggest early spay/neuter may influence cancer risk in certain breeds—talk to your vet about individualized timing. - Choose Reputable Breeders:
Ethical breeders screen for hereditary conditions and avoid breeding dogs with histories of aggressive cancers.
Prevention isn’t foolproof—but awareness gives you a powerful edge.
Frequently Asked Questions
Are mast cell tumors on the ear flap more dangerous?
Not necessarily—but their location makes complete surgical removal harder, potentially increasing recurrence risk if margins aren’t clean.
Can a mast cell tumor disappear on its own?
Rarely. Some MCTs may shrink temporarily with antihistamines or steroids, but they almost always return without definitive treatment.
How fast do mast cell tumors grow on the ear?
It varies: Grade I tumors may stay small for months, while Grade III can double in size within days or weeks.
Is my dog in pain from an ear flap MCT?
Often not initially—but as the tumor grows, ulcerates, or causes itching, discomfort increases. Head shaking or ear sensitivity are clues.
What’s the survival rate for dogs with ear MCTs?
With complete removal of a low-grade (Grade I) tumor, survival can exceed 90% at 2 years. High-grade or metastatic cases require aggressive therapy and have guarded prognosis.
Final Thoughts – Knowledge Is Your Dog’s Best Defense
A mast cell tumor on your dog’s ear flap is serious—but not hopeless. With modern diagnostics, tailored treatments, and vigilant aftercare, many dogs go on to live full, happy lives. What matters most is acting quickly, seeking expert guidance, and refusing to dismiss a “small bump” as nothing. Your attentiveness could make all the difference between early intervention and advanced disease. Trust your instincts, partner with your veterinary team, and remember: even in the face of cancer, love, care, and informed choices light the path forward.
Pemphigus Erythematosus in Cats: Best 7 Expert Tips! – Learn to recognize symptoms, manage flare-ups, and improve your cat’s quality of life.
Pemphigus Erythematosus in Dogs: Best 7 Expert Tips! – Discover causes, symptoms, and treatment options to manage this autoimmune skin condition effectively.
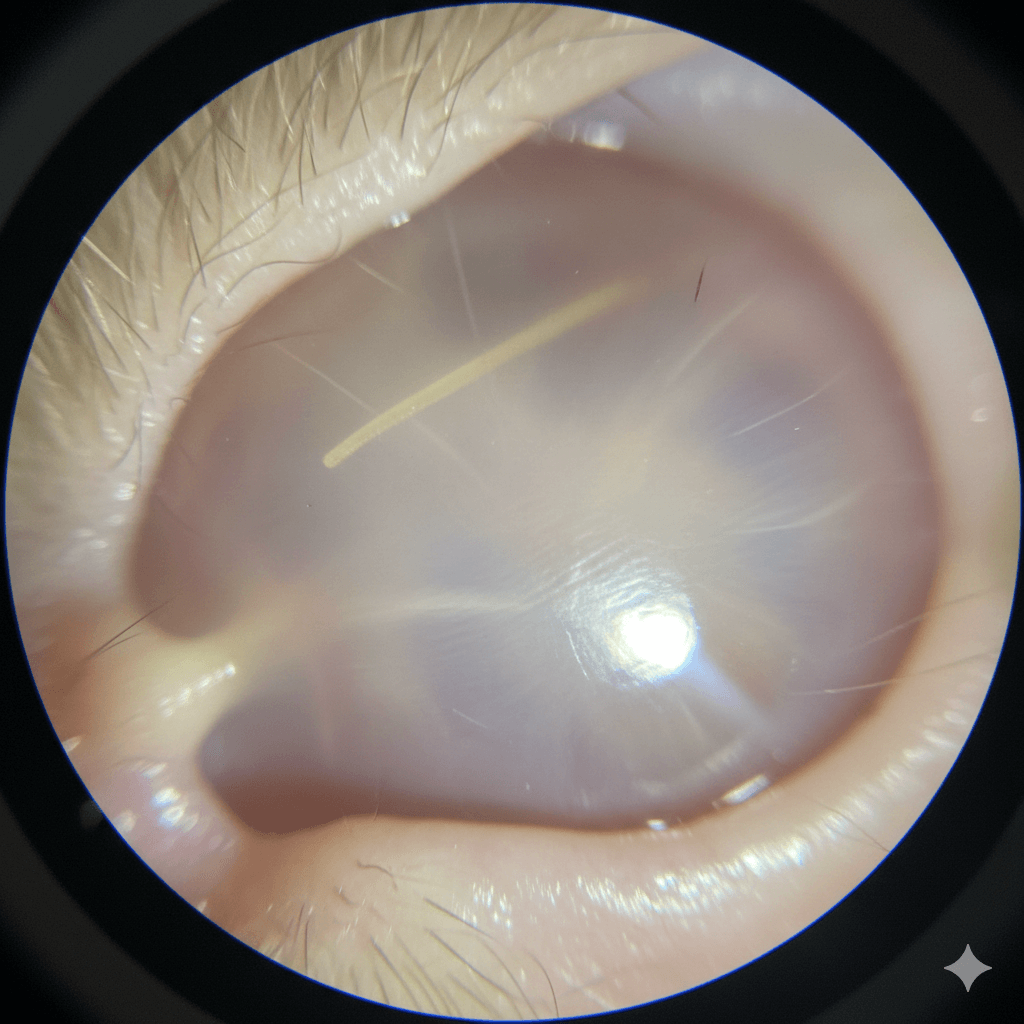
Cat Tympanic Membrane: Best 7 Expert Tips! – Learn how to protect your cat’s eardrum, spot issues early, and ensure lifelong auditory health.
Dog Tympanic Membrane: Best 7 Expert Tips! – Learn how to protect your dog’s eardrum, spot issues early, and ensure lifelong ear health with expert advice.