Hepatic Encephalopathy in Dogs: When the Liver Fails the Brain
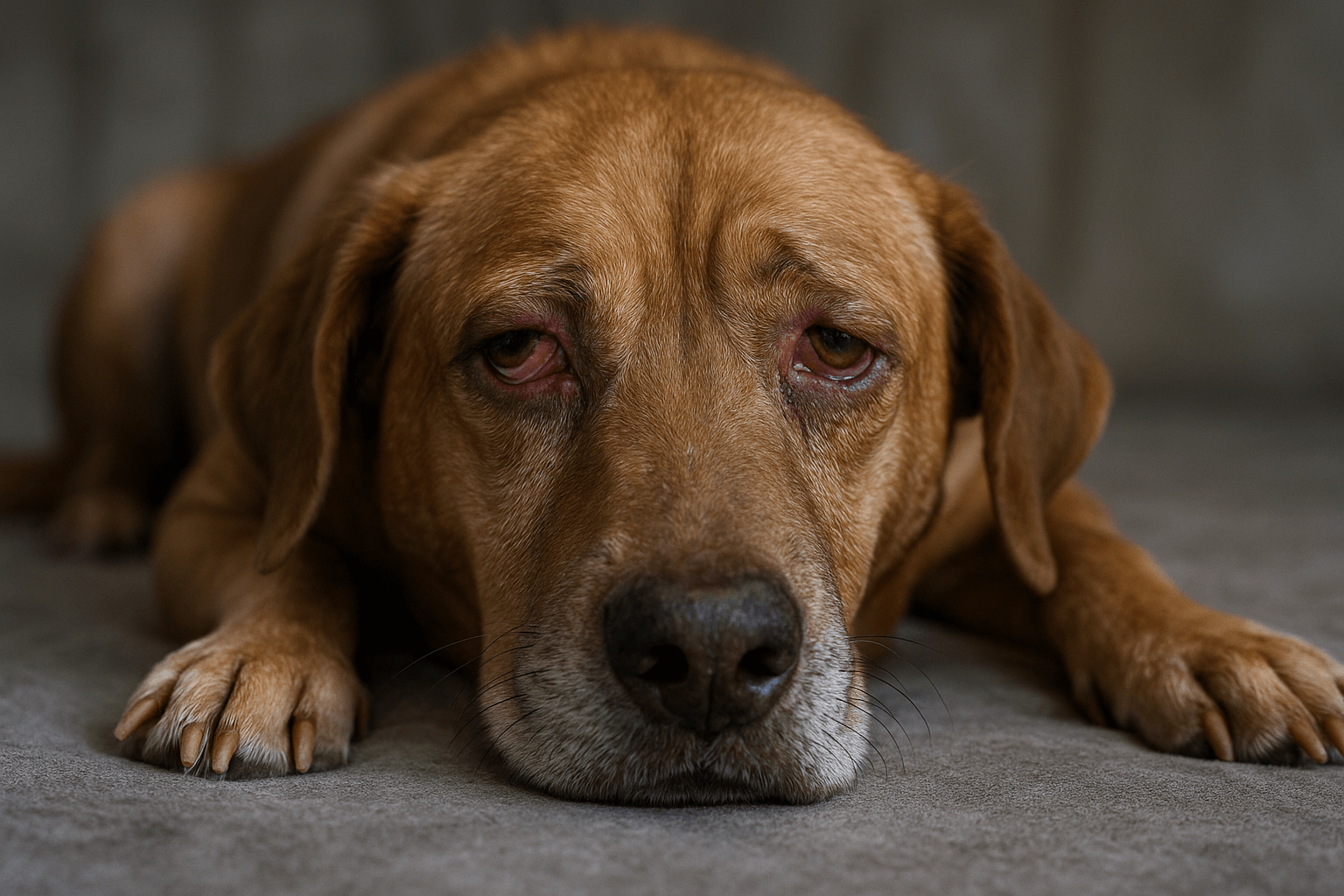
When a dog’s liver can’t filter toxins, the brain pays the price. Hepatic encephalopathy isn’t just a complication—it’s a neurological emergency masked as confusion, wobbling, or strange behavior. Many pet owners mistake these signs for aging or a “funny phase.” But behind the silence is a body in crisis. Understanding hepatic encephalopathy in dogs means recognizing the invisible battle happening inside—and acting before it’s too late.
What Hepatic Encephalopathy Really Is
Hepatic encephalopathy (HE) is not a disease on its own—it’s a neurological syndrome triggered by liver dysfunction. When the liver fails, ammonia and other toxins build up in the bloodstream and cross into the brain, disrupting normal function. Here’s why this happens:
Toxin Overload:
The liver normally breaks down ammonia from digested protein. In HE, it can’t keep up, and ammonia floods the brain.Portosystemic Shunts:
Some dogs are born with abnormal blood vessels that bypass the liver, letting toxins flow straight to the brain.Liver Disease Progression:
Chronic conditions like cirrhosis, hepatitis, or tumors damage liver tissue, reducing its filtering capacity.Triggering Factors:
Infections, constipation, high-protein meals, or certain medications can suddenly worsen toxin levels.Neurological Disruption:
Ammonia interferes with neurotransmitters, causing brain cells to swell and function abnormally.
This isn’t a slow decline—it’s a cascade. The brain doesn’t just “get tired.” It’s being poisoned. Recognizing the early signs can mean the difference between recovery and irreversible damage.

Common Signs of Hepatic Encephalopathy in Dogs
The symptoms of HE can be subtle at first—easily mistaken for lethargy or old age. But they escalate quickly. Pay close attention to these red flags:
Disorientation or Staring into Space:
Your dog may seem lost in familiar places, as if they’ve forgotten where they are.Head Pressing:
Pressing the head against walls, furniture, or corners is a classic and alarming sign of brain pressure.Circling or Pacing Repeatedly:
Compulsive, aimless movement without purpose signals neurological dysfunction.Seizures or Muscle Twitches:
Uncontrolled jerking, stiffness, or full-body convulsions indicate advanced brain involvement.Lethargy or Unresponsiveness:
A sudden drop in energy, ignoring commands, or appearing “zoned out” is not normal laziness—it’s neurological shutdown.
These behaviors aren’t quirks. They’re neurological alarms. If you notice even one of these signs, especially in a dog with known liver issues, seek veterinary care immediately. Delaying can cost you precious time.
Check this guide 👉Thiamine Deficiency in Dogs: Best 7 Expert Tips!
Check this guide 👉Understanding Myopathy in Dogs: Best 7 Expert Tips!
Check this guide 👉Symptoms of Liver Cancer in Dogs: Best 7 Expert Tips!
| Clinical Signs of Hepatic Encephalopathy | Underlying Mechanism |
|---|---|
| Head pressing against objects | Increased intracranial pressure from brain swelling due to ammonia toxicity. |
| Ataxia (wobbly gait, stumbling) | Neurotransmitter imbalance affecting motor coordination and balance centers. |
| Excessive drooling or difficulty swallowing | Neuromuscular impairment from toxin-induced nerve dysfunction. |
| Changes in personality or aggression | Frontal lobe disruption alters emotional regulation and impulse control. |
| Coma or unresponsiveness in late stages | Severe ammonia toxicity suppresses brainstem function and consciousness. |
Causes: Why Some Dogs Are More at Risk
Not all dogs develop hepatic encephalopathy. Certain breeds, conditions, and genetic factors make some far more vulnerable.
Congenital Portosystemic Shunts (PSS):
Common in small breeds like Yorkshire Terriers, Maltese, and Poodles—abnormal blood vessels bypass the liver from birth.Acquired Liver Disease:
Chronic hepatitis, cirrhosis, or liver tumors in older dogs (especially Cocker Spaniels, Dobermans) impair detoxification.High-Protein Diets:
Excess protein increases ammonia production—dangerous if the liver can’t process it.Gastrointestinal Issues:
Constipation, diarrhea, or intestinal bleeding increase toxin absorption into the bloodstream.Infections or Stress:
Fever, UTIs, or surgery can trigger a sudden worsening of HE in dogs with underlying liver problems.
Knowing your dog’s breed history and health background helps you anticipate risk. A puppy with a shunt needs different monitoring than an elderly dog with liver inflammation—but both need vigilance.
Diagnosis: How Vets Identify Hepatic Encephalopathy
There’s no single test for HE. Diagnosis requires piecing together clinical signs, lab results, and imaging. Here’s how it’s done:
Blood Work:
Elevated ammonia levels, low blood urea nitrogen (BUN), and abnormal liver enzymes are key indicators.Bile Acid Test:
Measures liver function by comparing bile acids before and after eating—abnormal results suggest poor detoxification.Ultrasound or CT Scan:
Reveals structural issues like shunts, tumors, or liver shrinkage.Neurological Exam:
Vets assess reflexes, mental status, and coordination to rule out other brain disorders like epilepsy or tumors.Response to Treatment Trial:
If symptoms improve with lactulose or a low-protein diet, HE is strongly suspected.
Early diagnosis is critical. Many dogs are misdiagnosed with “old age” or “seizure disorder” until their condition deteriorates. Don’t accept vague answers—push for comprehensive testing.
Treatment: Managing Hepatic Encephalopathy in Dogs
HE is manageable—but not curable—without addressing the root cause. Treatment is multi-layered and lifelong.
Dietary Modification:
Low-protein, high-quality diets reduce ammonia production. Special prescription foods like Hill’s l/d or Royal Canin Hepatic are often recommended.Lactulose Administration:
This sugar solution binds ammonia in the gut and promotes its excretion through stool—often the first-line treatment.Antibiotics (e.g., Metronidazole):
Reduce ammonia-producing bacteria in the intestines.Supportive Care:
IV fluids, anti-nausea meds, and seizure control drugs stabilize the dog during acute episodes.Surgery for Shunts:
In congenital cases, surgical correction of the abnormal vessel can be curative—especially in young dogs.
Treatment isn’t one-size-fits-all. A puppy with a shunt may need surgery. An older dog with cirrhosis may require lifelong medication and diet control. The goal? Keep toxins low, support liver function, and maintain quality of life.
Prognosis and Long-Term Management
The outlook depends on the cause, how early treatment begins, and how strictly the regimen is followed.
Congenital Shunts (Surgically Corrected):
Many dogs live normal, healthy lives after successful surgery—especially if treated before neurological damage occurs.Acquired Liver Disease:
Prognosis is guarded. With strict management, some dogs live for years. Without it, decline is rapid.Diet Compliance Is Non-Negotiable:
Even one high-protein treat can trigger a crisis. Every meal matters.Regular Monitoring:
Blood tests every 3–6 months track ammonia levels and liver function.Watch for Triggers:
Constipation, infections, or stress can cause sudden relapses—even in stable dogs.
This isn’t a short-term fix. It’s a lifestyle shift. But with consistency, many dogs enjoy happy, active lives—even with HE.
Prevention: What You Can Do Before It Starts
While some causes like congenital shunts can’t be prevented, you can reduce risks for others:
Avoid High-Protein Table Scraps:
No meat bones, chicken skin, or cheese. Stick to dog-safe, vet-approved treats.Keep Your Dog’s Bowels Regular:
Fiber-rich diets and daily walks prevent constipation—a major HE trigger.Schedule Annual Liver Screens:
Especially for at-risk breeds or older dogs—blood tests catch problems before symptoms appear.Avoid Toxins:
Keep medications, cleaning products, and pesticides away. The liver is your dog’s primary detox organ.Know Your Dog’s Baseline:
Learn what’s normal for your dog—energy levels, appetite, litter habits. Sudden changes are your earliest warning.
Prevention isn’t about fear. It’s about awareness. The best treatment is catching it before the brain is affected.
FAQ: Hepatic Encephalopathy in Dogs
Can a dog recover fully from hepatic encephalopathy?
Yes—if caused by a congenital shunt corrected surgically. If due to chronic liver disease, recovery means long-term management, not cure.
Is hepatic encephalopathy contagious?
No. It’s a metabolic disorder, not an infection. Other pets are not at risk.
How long can a dog live with hepatic encephalopathy?
With proper care, many live 1–5+ years. Without treatment, survival is often weeks to months.
Can I give my dog a regular dog food if they have HE?
Never. Standard kibble is too high in protein and can trigger a life-threatening crisis. Use only vet-prescribed diets.
My dog seems better after starting lactulose—can I stop the medication?
Absolutely not. Lactulose must be given daily, even if symptoms improve. Stopping abruptly causes rapid toxin buildup.
You Are Their Liver When Their Own Fails
Hepatic encephalopathy doesn’t announce itself with a bark or a whimper. It creeps in—quietly, deceptively—until your dog stares blankly at the wall, or presses their head into the floor as if trying to push the confusion away.
You won’t cure it with love alone.
But you can save them with knowledge.
With every low-protein meal.
With every scheduled blood test.
With every gentle hand guiding them to their bed when they’re too dizzy to stand.
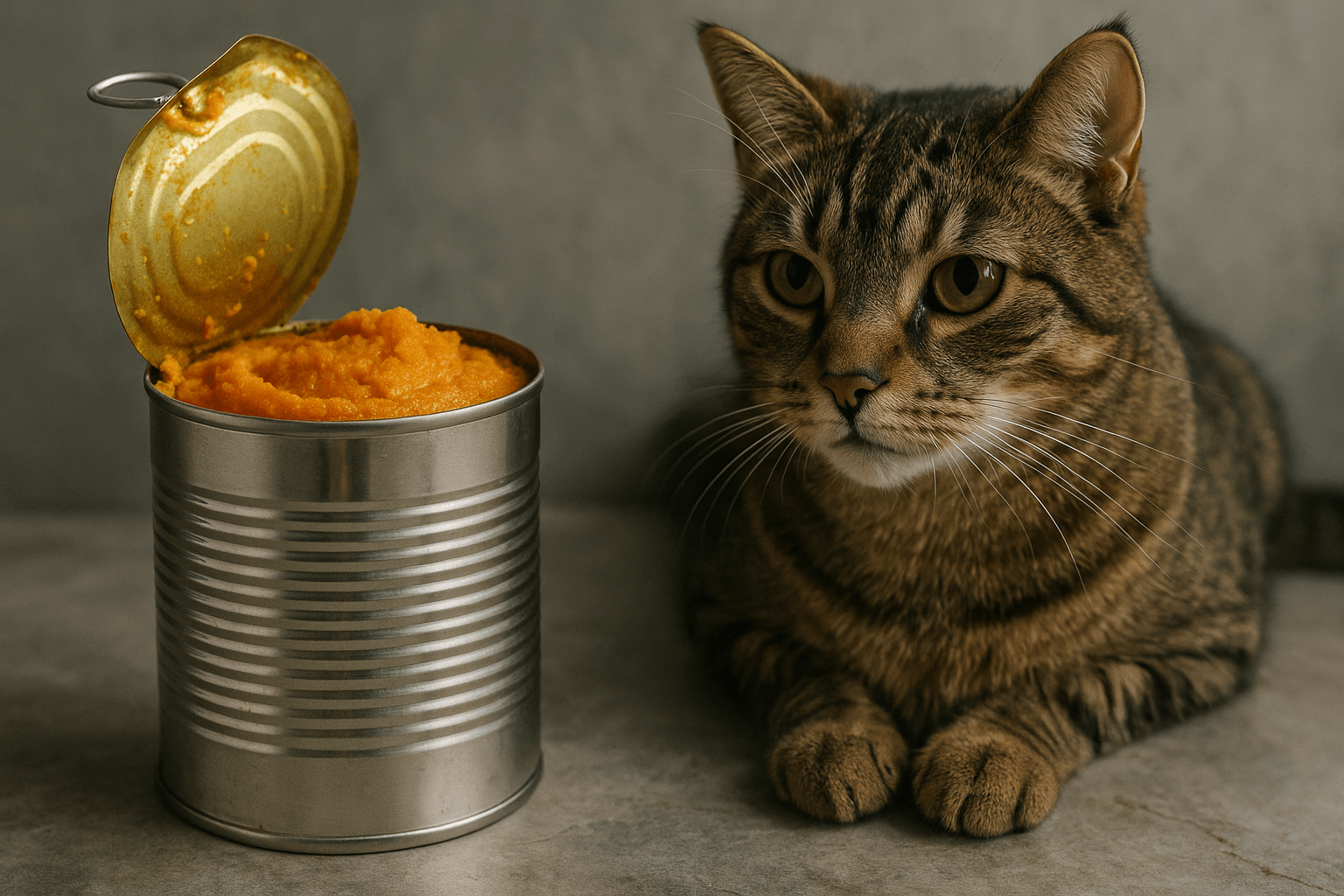
Canned Pumpkin for Cat Diarrhea: Best 7 Expert Tips! Natural remedy to firm stools, soothe upset bellies, and support gut health safely.
Can a Cat Give You Scabies? Best 7 Expert Tips! Discover the truth about feline mites, human skin risks, and how to protect yourself—without panic.
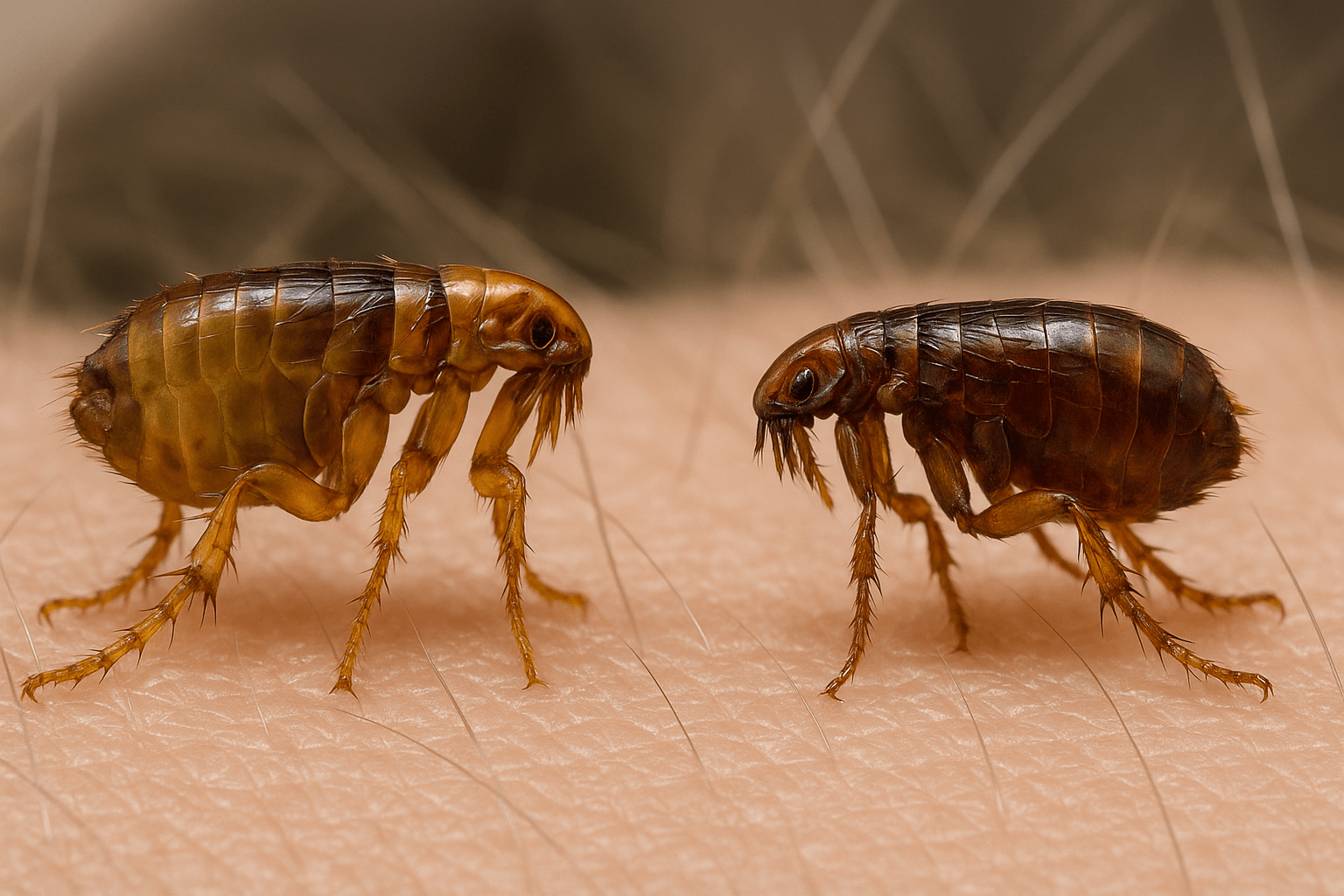
Cat Flea vs Human Flea: Best 7 Expert Tips! Discover the truth about bites, species, and how to eliminate infestations for good.
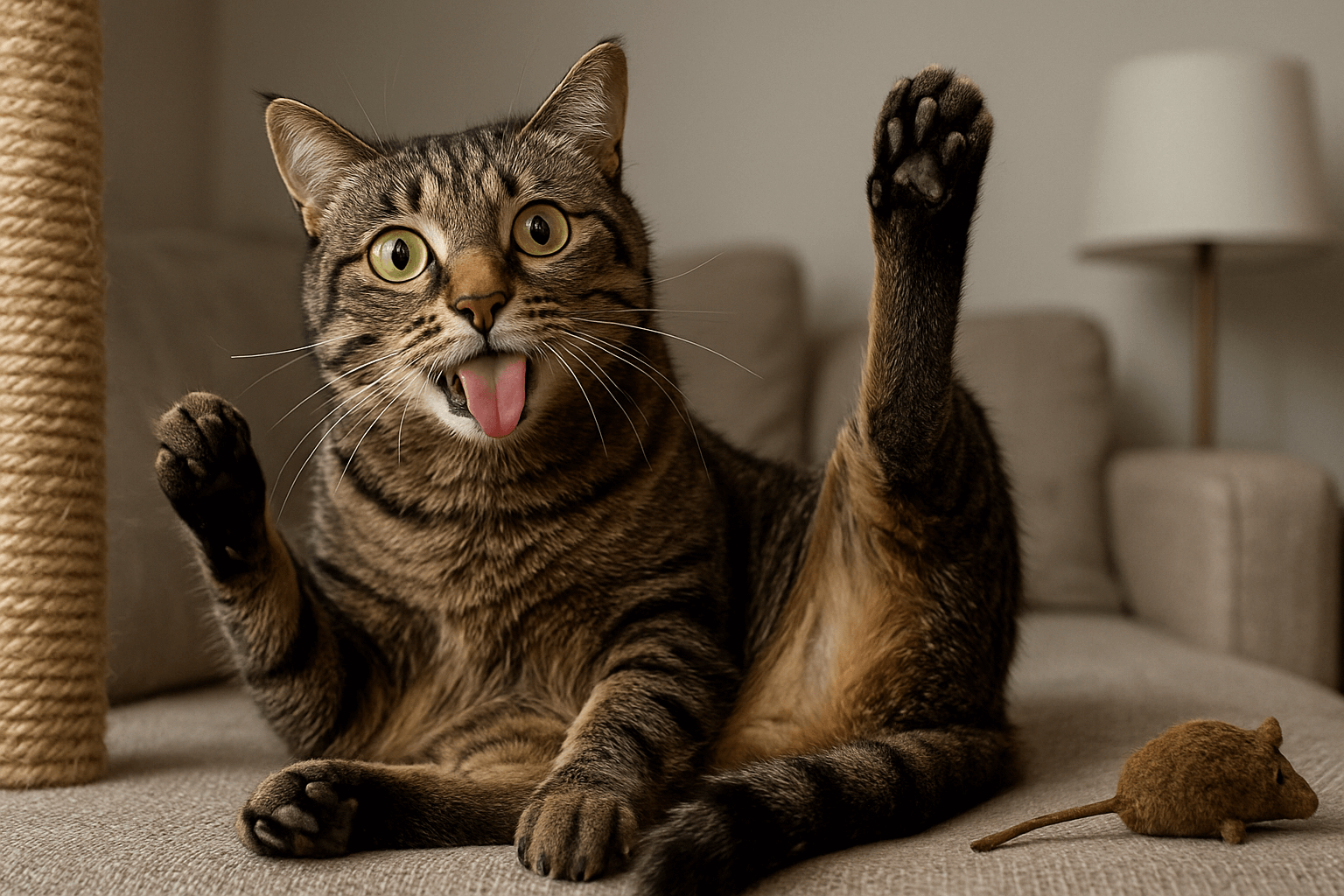
Weird Cat Behaviors: Best 7 Expert Tips! Discover why cats do strange things—and how to understand, not punish, their instincts for a happier home.